Medicinal cannabis is changing the face of clinical medicine. We are the leaders of that change.

























































At CED Clinic, we’re redefining care. Step into a welcoming, professional space where the leading experts in medical cannabis are here to guide and support you!

You’ve found the right place!


🔥 CED Clinic: voted Best Medical Cannabis Clinic since 2013!

Our Services
- Expert Telemedicine Medical Cannabis Consultations!
- Medical Card Certifications (Massachusetts, New Hampshire, Rhode Island, Vermont, Maine)
- Adult Cannabis Care (Everyone in the US + Internationally)
- Pediatric Cannabis Care (Everyone in the US + Internationally)
- In-Depth Consultations & Care Plans
- Personalized Services (Medication, Diagnostic, and Management Review)
- Cannabis and Non-Cannabis Medical Second Opinions
- Long-term Talk Therapy
- Advice, Support, and Cost-Savings Advice!
Our Mission
- To Heal
- To Listen
- To Educate
- To Learn and Understand
Questions? 👉 Contact Us Here
Our Team
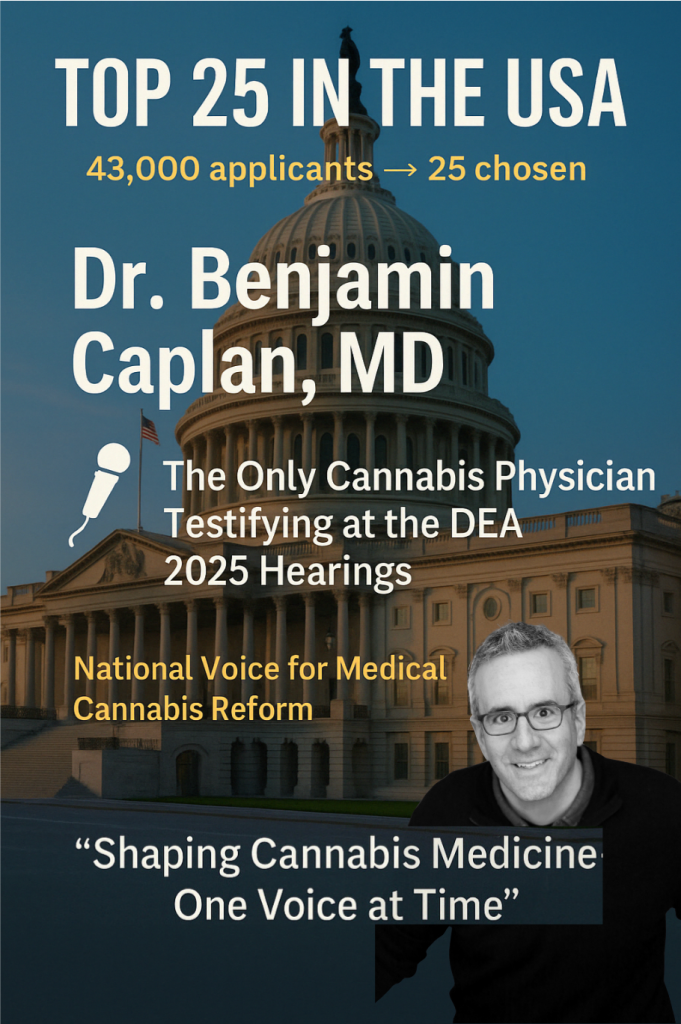
Benjamin Caplan, MD, stands at the forefront of medical cannabis care as the Founder and Chief Medical Officer of CED Clinic and CED Foundation. His entrepreneurial journey further extends as the Founder of multiple medical cannabis technology and educational platforms and as a medical advisor to the prestigious cannabis investment fund, GreenAXS Capital. Within digital healthcare, Dr. Caplan co-founded EO Care, Inc, a pioneering digital therapeutic and telemedicine platform, offering personalized cannabis care and product plans and continuous clinical guidance to a global clientele seeking a reliable, evidence-based cannabis care partner. Adding to his repertoire of contributions to the medical cannabis arena, Dr. Caplan has recently published “The Doctor-Approved Cannabis Handbook,” an industry-first resource empowering readers with the full scope of the therapeutic potential of cannabis. Through his multifaceted involvement, Dr. Caplan continuously strives to bridge the gap between traditional medicine and cannabis care, making a significant impact in evolving holistic healthcare.
Erin Caplan, NP is a board-certified Pediatric Nurse Practitioner with a master’s-level medical education from Simmons. Her extensive clinical journey has been enriched through roles at Massachusetts General Hospital, Hyde Park Pediatrics, Atrius Healthcare, and Dana-Farber Cancer Institute, where she has provided both inpatient and outpatient primary care to some of the most fragile and challenging pediatric patients. A registered cannabis care provider licensed by the Massachusetts Cannabis Control Commission, Erin seamlessly blends her pediatric expertise with the nuance and adaptability required for personalized cannabis care. A community leader, avid athlete, and dedicated mother of four, Erin’s compassionate bedside manner and steadfast commitment to evidence-based practice have earned her the trust and appreciation of patients and families, showcasing her as a harmonious blend of clinical excellence with a personal touch.
Patient Stories
Navigating the Stigma as a Senior
Testimonial:
“At 68 years old, I never thought I’d be considering cannabis as part of my treatment. My generation didn’t grow up viewing it as medicine—we saw it as something entirely different. But after dealing with arthritis pain for over a decade, my daughter encouraged me to give it a try. Meeting with a professional who truly understood both the science and the hesitations I had made all the difference. Dr. Caplan explained how cannabis could work alongside my existing treatments and offered me a gradual approach to build my confidence. Now, I’m using a tincture daily, and I feel a level of relief and mobility that I hadn’t felt in years. Even better, I’ve been able to have open conversations with my friends about the benefits, helping them see it in a new light too.”
Peter H
Reclaiming Life with Holistic Care
“I had been living with chronic fatigue for years, feeling like I was just existing rather than living. Traditional medicine had brought little relief, so I started looking into alternative options. Working with a doctor who truly listened to my struggles and offered a holistic approach to care was a game-changer. The cannabis regimen we developed not only improved my energy levels but also allowed me to engage in activities I hadn’t been able to enjoy in years. This isn’t just about managing symptoms—it’s about reclaiming a life I thought was out of reach. I’m grateful for the guidance and the opportunity to feel like myself again.”
Sarah M
A Patient’s Guide to Finding the Right Dose
“My journey with cannabis therapy was not a straight line. When I first started, I thought one dose or product would fix everything, but I quickly learned it’s a process of trial and adjustment. Working with a knowledgeable doctor made all the difference. We started low and slow, as they say, and I kept track of how I felt each day. Over time, I found the right balance that worked for my condition without unwanted side effects. The best part of this process was how involved I felt—I wasn’t just following instructions; I was an active participant in my own care. Now, I’m managing my symptoms better than ever and feel in control of my health.”
Michael T
Finding Balance After Postpartum Anxiety
“After having my second baby, I struggled with severe postpartum anxiety. It was difficult to admit I wasn’t feeling okay, and even harder to ask for help. Traditional treatments left me feeling disconnected and foggy, and I didn’t want to spend my days like that. When I started exploring medical cannabis, I was cautious but hopeful. Meeting with a knowledgeable doctor helped me approach it with confidence. I started with a low dose of CBD and gradually added a small amount of THC for nighttime use. Within weeks, I noticed a difference—not just in my anxiety, but in my ability to enjoy motherhood again. This journey wasn’t just about managing symptoms; it was about regaining balance and finding joy in my life.”
Emily R
New Hope for Fibromyalgia
“I never thought I’d find a doctor who could make me feel optimistic about managing my fibromyalgia, but Dr. Caplan did exactly that. He didn’t just focus on symptoms—he helped me think about my health in a holistic way, integrating cannabis into a broader plan for wellness. His recommendations were precise, and he made sure I knew how to adjust them as needed. What really impressed me was his dedication to follow-up care; he personally checked in to see how I was doing and offered adjustments based on my progress. It’s that level of personalized attention that makes Dr. Caplan and his clinic stand out.”
Grace N
Overcoming My Fear of Cannabis Therapy
“For years, I hesitated to explore medical cannabis. I had so many misconceptions—fear of side effects, worries about legality, and even embarrassment about what others might think. But after years of struggling with my chronic anxiety, I decided it was time to explore new options. Meeting with Dr. Caplan completely shifted my perspective. He helped me understand that cannabis wasn’t about masking symptoms; it was about restoring balance in a way that felt right for me. My first steps were small, and we adjusted the plan together over time. Today, I feel a sense of calm and clarity I hadn’t thought possible. More importantly, I’ve let go of the stigma and feel proud of my decision to prioritize my health.”
Julia M
Care That Transcends Expectations
“Dr. Caplan’s clinic is a masterclass in patient care. From the moment you step in, you feel like you’re in capable, compassionate hands. He took the time to understand my chronic fatigue and explained how cannabis could help in ways I hadn’t considered. What stood out most was his emphasis on making informed decisions—he’s not just a doctor, but a teacher who ensures you leave with a clear understanding of your treatment. His book is a fantastic resource, and it was clear from our discussion that he truly believes in empowering his patients through education. I couldn’t be happier with my experience.”
Daniel R
The Expert You Can Trust
“Dr. Caplan’s reputation as a cannabis expert is well-earned. I came to him with a list of concerns about using cannabis for my autoimmune condition, and he addressed each one with patience and expertise. He went beyond the surface to help me understand not just the benefits but also potential risks, which made me feel secure in my treatment. His recommendations were so thoughtful and practical, and he even tailored them to fit my busy schedule. What really set him apart, though, was his genuine care—I could tell he wanted me to succeed in managing my health. It’s rare to find a doctor who combines this level of expertise with such a warm, approachable demeanor.”
Sophia L
Empowering Through Education
“As a mother of two, I was cautious about trying medical cannabis for postpartum anxiety, but Dr. Caplan quickly put my fears at ease. He offered a science-backed approach that felt safe and sensible, walking me through each step with empathy and care. His book was also an invaluable tool—it gave me the confidence to understand how to approach treatment without guesswork. Now, I feel like I’m thriving instead of just surviving. I’m so grateful for Dr. Caplan’s guidance and for the way he made this process feel not only accessible but also empowering.”
Olivia G
Clearer Days Ahead
“After years of chronic migraines and no relief from traditional treatments, I turned to Dr. Caplan as a last resort. What I found was a doctor who genuinely listened to my struggles and worked with me to find solutions. His clinic is a beacon for anyone looking to explore medical cannabis with confidence. He didn’t just give me a prescription—he educated me about dosing, timing, and the different products available. His insights were life-changing, and his approachable manner made even the complicated aspects of treatment easy to understand. For anyone hesitant about this path, Dr. Caplan is the guide you’ve been waiting for.”
Ryan T
Game-Changer for Mental Health
“Finding Dr. Caplan was a game-changer for my mental health. For years, I struggled with anxiety and sleep issues, trying countless medications with limited success. Dr. Caplan’s personalized approach was a breath of fresh air. He didn’t just focus on my symptoms; he wanted to understand how my lifestyle and goals factored into the equation. His guidance helped me find a regimen that not only improved my sleep but also reduced my daily stress. The best part? He checked in after a few weeks to make sure everything was working smoothly. I’ve never felt so cared for by a doctor.”
Emily P
A Senior’s New Hope
“As a senior struggling with arthritis, I was skeptical about cannabis therapy. But Dr. Caplan changed my perspective completely. His extensive knowledge, combined with a genuine compassion for his patients, made my first visit feel like a turning point. He introduced me to options that were gentle and easy to integrate into my daily life. What surprised me most was how much he emphasized education—his book became a valuable resource for me and my family to better understand how cannabis could help. If you’re new to this world, Dr. Caplan is the expert you can trust to guide you with care and patience.”
Lucas H
Skeptic to Believer
“I had given up on finding relief for my chronic pain until I met Dr. Caplan. His calm, reassuring demeanor put me at ease from the moment we sat down. He not only prescribed a cannabis regimen tailored to my needs but also took the time to address my fears about stigma and side effects. What made the experience even better was how he explained things—breaking down complex science into simple, relatable examples. I now feel in control of my health for the first time in years. If you’re hesitant about exploring cannabis as an option, Dr. Caplan’s patient-centered care will make all the difference.”
Chloe M
Revolutionizing My Care
“Dr. Caplan’s approach to cannabis therapy is revolutionary. I had been to other clinics where the process felt rushed and impersonal, but my experience with him was the exact opposite. He asked thoughtful questions, delved into my medical history, and crafted a tailored plan to address my specific symptoms. What stood out the most was his ability to connect my condition to real-world cannabis applications, referencing research and patient success stories that inspired confidence. His clinic also provides resources beyond the appointment—like follow-ups and his book—which made me feel supported every step of the way. For anyone seeking a truly personalized and informed approach to medical cannabis, I can’t recommend Dr. Caplan enough.”
Ethan K
Trust Built Through Understanding
“Trust is not something I give easily when it comes to my healthcare, but Dr. Caplan earned it during our first appointment. He listened carefully to my concerns and explained the science behind medical cannabis in a way that was clear and accessible. He didn’t just focus on the benefits; he also made sure I understood potential challenges and how to navigate them. That kind of transparency and care is rare, and it’s the reason I feel confident in the treatment plan we developed together.”
Emily C
Personalized Care That Stands Out
“Every aspect of my experience with Dr. Caplan reflected his commitment to personalized care. He took the time to ask about my lifestyle, my goals, and even my hesitations about using medical cannabis. His thoughtful questions and detailed explanations made it clear that he was focused on creating a plan that would work for me specifically. I also appreciated how he checked in with me after the visit to see how I was doing—a small gesture that made a big difference in my confidence and comfort moving forward.”
Olivia H
Educational and Empowering
“Dr. Caplan doesn’t just prescribe cannabis—he educates you about it, so you feel confident and in control of your treatment. From our first appointment, it was clear that he cared about making sure I understood all my options. He referenced research, shared stories from other patients, and even recommended chapters from his book that were particularly relevant to my situation. By the end of the visit, I felt not only more informed but also more empowered to make decisions about my health. That kind of care is rare, and I’m grateful for it.”
Benjamin R
Clear Guidance Every Step of the Way
“What struck me most about Dr. Caplan was his ability to provide clear and actionable guidance. I had no prior experience with medical cannabis and was overwhelmed by all the information out there, but he made it manageable. He walked me through the options, explained the potential benefits and risks, and helped me navigate decisions in a way that felt completely tailored to my situation. His calm and thoughtful manner put me at ease, and I left the appointment feeling like I finally had a plan I could trust.”
Chloe M
A Tailored and Thoughtful Plan
“Dr. Caplan approached my case with a level of care and detail I hadn’t experienced before. Instead of a one-size-fits-all recommendation, he tailored a plan based on my specific symptoms and preferences. He took the time to explain why certain options might work better for me and made sure I felt comfortable moving forward. His advice was practical and grounded in science, yet delivered in a way that felt approachable. I left feeling empowered, knowing I had the tools and knowledge to take the next steps with confidence.”
Ethan K
More Than Just a Weed Visit
“My first visit with Dr. Caplan felt like more than just a routine medical appointment—it was an opportunity to truly take charge of my health. He asked questions that no other doctor had asked and encouraged me to think about my goals for treatment in a way I hadn’t before. His book was an incredible resource, but what truly set him apart was his ability to make the information feel relevant to my unique situation. I felt supported not only as a patient but as a partner in my healthcare journey.”
Maria L
A Practical and Supportive Approach
“Dr. Caplan’s approach is refreshingly practical and supportive. During our consultation, he focused not just on recommending cannabis, but on helping me understand how to use it in a way that fit my lifestyle and goals. He walked me through options, shared insights from his book, and even helped me think through how to manage dosing and timing. What really impressed me was his focus on the long term—this wasn’t about a one-time solution but about creating sustainable improvements in my health. It’s rare to find a doctor who invests this level of thought and care into patient guidance.”
John W
Dr. Caplan’s Expertise and Patience
“I was initially unsure about whether medical cannabis was the right path for me, but Dr. Caplan quickly put my concerns to rest. He spent time understanding my medical history and current challenges, carefully explaining the science behind cannabis and how it could fit into my treatment plan. His depth of knowledge and ability to communicate complex concepts in simple terms stood out to me. I appreciated his patience, especially when I had a list of questions, all of which he addressed thoroughly. The care I received was thoughtful and personalized, and I left feeling confident in the steps we outlined together.”
-Sophia R
A Lighthouse in the Storm
“When I first started exploring medical cannabis, I felt overwhelmed by conflicting advice online. Meeting Dr. Caplan was like finding a lighthouse in a storm. He didn’t just recommend a treatment plan; he broke down every step, explaining the science in plain terms so I could make informed decisions. His book, ‘The Doctor-Approved Cannabis Handbook,’ became my go-to guide between visits. It’s rare to find a doctor who takes so much time to ensure you feel educated and empowered. Now, not only am I managing my symptoms, but I feel like I truly understand my body better. If you’re looking for compassionate care and clear guidance, Dr. Caplan is the doctor you need.”
Sophia J
I Finally Got My Stress Under Control
I used to pride myself on being able to handle anything work threw at me. Long hours, tight deadlines, a demanding boss—it was all part of the game, and I thought I had it down. But somewhere along the way, the stress started to build up. Slowly at first, then all at once. I was losing sleep, snapping at my family, and my chest constantly felt tight. The smallest things would set me off, and no amount of weekends or ‘self-care’ could fix it. I didn’t recognize myself anymore.
My doctor had suggested anti-anxiety meds, but I didn’t want to go that route. I kept thinking, there’s got to be another way. A friend mentioned cannabis, and I’ll admit, I laughed at first. Cannabis? For work stress? I thought it was a joke. But after another sleepless week and two missed deadlines, I was willing to try anything. That’s when I found CED Clinic and Dr Caplan.
I wasn’t sure what to expect going in, but Dr. Caplan made me feel comfortable right away. He listened—not just to what I was saying, but to what I wasn’t saying, if that makes sense. He didn’t treat me like a case file or just another patient. We talked about the stress, sure, but also about why I’d been so hesitant to ask for help. He suggested a low-dose CBD regimen to help me unwind without feeling ‘off,’ and explained that it wasn’t about numbing out—it was about finding balance again.
It took a few weeks before I really started noticing a difference. At first, I wasn’t sure if it was doing anything, but then I realized I wasn’t lying awake at night, going over work problems in my head. I wasn’t clenching my jaw every time I opened an email. The stress didn’t go away, but I wasn’t drowning in it anymore. I felt like I could handle things again, like the weight had been lifted just enough for me to breathe.
Now, I can get through my workday without feeling like I’m on the verge of a meltdown. I’m more present with my family, more patient. It’s not perfect, and work is still stressful, but it doesn’t own me anymore. I can’t say enough about what Dr. Caplan did for me. I was lost, and he helped me find my way back.”*
– Jason B
Our Son Found Calm, and So Did We
Our son has always been… difficult, to put it lightly. He’s smart, no doubt about that, but for as long as I can remember, we’ve struggled with his defiance. It was like every day was a battle—he’d talk back, refuse to listen, and disrupt everything at home and at school. We’d get calls from his teachers constantly about how he couldn’t sit still or follow directions. He was failing classes, not because he didn’t understand the material, but because he just refused to engage. I started to feel like we were losing control, not just of him, but of our family. It was exhausting. We tried everything—therapy, behavior charts, punishments, rewards—but nothing seemed to get through to him.
When someone suggested we look into cannabis, I’ll admit, I was pretty skeptical. The idea of giving our son cannabis? It felt like too much. But at the same time, I felt like we were running out of options. I mean, we couldn’t keep going the way we were. So, I did some research and found Dr. Caplan. I didn’t really know what to expect, but I figured it was worth at least hearing what he had to say. When we met with him, Dr. Caplan was so calm, so understanding. He didn’t make us feel like we were bad parents, which, honestly, was a huge relief. We’d been feeling like failures for a long time. He explained that cannabis, in the right doses, might help our son relax, become more receptive, and just… chill out.
At first, I wasn’t sure. But we decided to give it a shot because we needed something to change. I remember the first few weeks—we were waiting for a miracle that didn’t come right away. But slowly, things started to shift. He wasn’t perfect, and I didn’t expect him to be, but we started seeing moments of calm, of compliance. He’d sit down and actually listen when we talked to him. His teachers noticed, too. The calls home weren’t as frequent, and when they did call, it wasn’t about him disrupting the class, but little moments where he was making an effort. He wasn’t fighting us over every single thing anymore. He even started being more responsible around the house—little things like cleaning up after himself, finishing homework without a meltdown.
It wasn’t an overnight transformation, but it was enough to make us believe that maybe—just maybe—things could get better. And they have. Our son is still a work in progress, but aren’t we all? He’s more in control now, more aware of his actions. I can’t tell you what a relief it is to have peace in our home again, even if it’s not perfect all the time. We can breathe. We can plan things without the constant fear of a blow-up. Dr. Caplan gave us the space to feel like parents again, instead of just referees in constant battles.
– Heather R.
Finally Found Relief from Menopause
Menopause hit me like a freight train. One minute I was fine, and the next, I was drowning in hot flashes, mood swings, sleepless nights, and constant irritability. It felt like I couldn’t get through the day without snapping at someone or dripping in sweat. The worst part was the lack of sleep—I’d toss and turn all night, then drag myself through the day feeling exhausted. It was like I had no control over my own body, and everything just felt harder. I tried the usual over-the-counter remedies and even considered hormone replacement therapy, but I didn’t like the risks. Honestly, I was starting to lose hope.
A friend of mine, who had been seeing Dr. Caplan for her own health issues, suggested I give him a try. I wasn’t sure at first. Cannabis for menopause? It seemed a little out there. But after trying everything else and getting nowhere, I figured I had nothing to lose. From the moment I met with Dr. Caplan, I knew I was in the right place. He listened to all my complaints without judgment—he understood how tough it was. He didn’t just hand me a one-size-fits-all solution either. Instead, he explained how cannabis could help balance out my mood swings, improve my sleep, and even ease the intensity of the hot flashes. He was thorough, but he kept it simple, so I didn’t feel overwhelmed.
Within a few weeks of starting on a low-dose regimen, I noticed a real change. The hot flashes were still there, but they weren’t as intense, and I wasn’t waking up drenched in sweat every night. My mood swings started to even out too. I wasn’t losing my temper over every little thing, and I was able to get through the day without feeling like I was on edge all the time. Most importantly, I started sleeping again. I’m not talking about perfect, uninterrupted sleep, but I was actually getting solid rest and waking up feeling more human. My irritability softened as my body felt more balanced.
I can’t say enough good things about Dr. Caplan and the care he’s given me. Menopause doesn’t feel like it’s running my life anymore. I have a handle on it now, and I feel like myself again. Cannabis wasn’t something I ever thought I’d turn to, but I’m so glad I did. Dr. Caplan gave me back my peace of mind, and for that, I’ll be forever grateful.
– Lisa M.
Cannabis Gave Us Our Family Back
“We live in California. Our son has severe autism, OCD, and behavioral issues that have ruled our lives for as long as I can remember. He struggles with communication, and when things don’t go as expected, the meltdowns are explosive. There are days when he self-injures so severely that I can’t leave him alone for a second. The screams, the head-banging, the constant pacing—it’s heartbreaking and terrifying. My husband and I have felt like prisoners in our own home. We can’t go shopping, we can’t take vacations, we can’t even break from the daily routine without risking an episode that could throw him into a spiral for weeks. We’ve tried every therapy, every medication. Nothing seemed to give him—or us—a moment of peace. It was draining every ounce of energy and hope we had left.
When someone first suggested cannabis to us, I was hesitant, scared even. I didn’t know how it would affect him. I see potheads and druggies everywhere these days in my area, and it does not look appealing. Would it help, or make things worse? But we were desperate, and a friend had read The Cannabis Handbook and suggested that we reach out, so we decided to see Dr. Caplan. I’ll never forget that first meeting. He listened—really listened—to the hell we’ve been living through, and for the first time in a long time, I felt like someone understood. His questions made it clear that he’s been through this with many others. He seemed to get our struggle like no doctor I’ve ever encountered. He wasn’t dismissive, and he cetainly didn’t make us feel crazy for trying something new – the way all of my other doctors do. He explained how cannabis could help with the anxiety, the OCD, and even the self-injury, in a way that was calm and controlled, without overwhelming us. Our son came on camera with a tantrum, and Dr Caplan was as patient and attentive, supportive, as I wish docs all were. Dr. Caplan carefully walked us through everything, never pushing, always respecting our concerns. His focus is so clearly empowering us, not tripping on himself or being on high.
We started our son on small doses of a few products, and I won’t lie, it wasn’t a quick, overnight change. But over time, with adjustments that he oversaw with us, we saw it—he started to calm down. The meltdowns weren’t as frequent, and when they did happen, they didn’t last as long or get as intense. The self-injury started to lessen. It felt like we could breathe again, like we had a little more room to live. We’re still careful—routine is still important—but the constant terror of something going wrong isn’t hanging over our heads as much. For the first time in years, my husband and I were able to go out for dinner. It sounds like such a small thing, but it was a moment where we could remember what life used to be like, before we became prisoners to our son’s condition.
I can’t say that cannabis has fixed everything, but it’s given us something we didn’t have before: hope. We’re seeing glimpses of who our son is underneath the anxiety and the behavioral issues. Dr. Caplan’s patience and understanding have been a lifeline for us. He gave us a way to manage our lives again. We’re still on this journey, but for the first time, it feels like there’s light at the end of the tunnel.”
– Sarah W.
Finding Comfort and Connection Again
“Loneliness had been creeping up on me for years, but it really hit hard when I retired. My social circle started shrinking, and the days just felt longer and emptier. I had been keeping busy with hobbies, but the silence in my house became unbearable. I’d wake up in the morning with no motivation to get out of bed because I didn’t have anyone to talk to, nowhere I really needed to be. I tried to reach out to old friends, but it always felt awkward, like I didn’t fit into their lives anymore. My primary doctor referred me to Dr. Caplan, not because of anything physical, but because they thought cannabis might help me with the emotional side of things. I was pretty skeptical. Cannabis? For loneliness? I didn’t see how it could possibly make me feel less isolated.
When I met with Dr. Caplan, he listened without judgment. I explained how I felt like I was drifting through my days, disconnected from everyone around me. He was calm and compassionate, and he didn’t rush me at all. Instead of dismissing my feelings, he talked me through how cannabis might help me not feel so ‘stuck’ in my emotions. We started with a low-dose regimen that focused on CBD to help with the feelings of overwhelm and helplessness. It wasn’t a quick fix, but after a few weeks, I noticed I felt lighter, more at ease. I found it easier to pick up the phone and call an old friend, easier to motivate myself to go out for a walk or run errands.
It’s hard to explain, but it felt like a weight had lifted off my chest. The loneliness was still there, but it didn’t feel so suffocating. I could breathe again, could start imagining a life where I wasn’t so isolated. Over time, I’ve been able to reconnect with people, even make new friends. Cannabis didn’t solve everything, but it gave me the space I needed to start living again. Dr. Caplan was there every step of the way, adjusting the treatment as we went and always making sure I was comfortable. I never thought something like this could help with how I was feeling, but I’m so glad I gave it a chance.”*
– Tom B.
Does Cannabis Work for Pediatric Autism? Yes!
“I wanted to take a moment to share a heartfelt message we recently received from one of Dr. Caplan’s patients. It’s moments like these that remind us why we’re so passionate about the work we do. The incredible progress described below is a testament to the power of personalized care and cannabis therapy. We’re grateful to witness such transformations and hope this story provides inspiration for others seeking hope and relief.”
– Jack Thompson, CED Clinic Operations Manager
For anyone interested in seeing Dr. Caplan as a consulting physician, please visit this link:Book an Appointment to complete our intake form, make a payment, and schedule your visit—all in one easy step.

Managing Anxiety with Cannabis: A Personal Story of Relief
“I heard about Dr. Caplan through a friend who had been his patient for a couple of years. I had been struggling with anxiety for a while but didn’t think cannabis was something I could handle. The stigma around it made me nervous, and I wasn’t sure it was for me. But my friend couldn’t stop raving about the difference Dr. Caplan had made in her life, so I finally decided to check him out. From the moment I sat down with him, I knew I was in good hands. He took the time to understand my situation, explaining how cannabis could be used to manage anxiety in a safe, controlled way. It wasn’t about pushing a product—it was about finding the right balance for my body and my needs. Now, I feel more in control of my anxiety than I have in years, and I’m grateful for Dr. Caplan’s thoughtful and thorough care.”
– Maria S.
Finally Found Relief for My Back Pain
“I was at my wit’s end with my lower back pain, and nothing seemed to work—painkillers, physical therapy, injections—you name it. My orthopedist mentioned Dr. Caplan, and honestly, I wasn’t sure about the whole cannabis thing. I mean, I wasn’t against it, but I didn’t think it was for me. Still, I was desperate, so I made the call. Dr. Caplan wasn’t like any other doctor I’d met. He really took the time to get to know me, my history, and my concerns about cannabis. He didn’t push anything but explained how it could help manage pain and inflammation in a way I could understand. He helped me feel like this was something worth trying, not some weird ‘last resort.’ Fast forward six months, and I’m moving around a lot better than I have in years. I never thought I’d say it, but cannabis has made a huge difference in my life. Dr. Caplan’s been there for every step, making sure I get the right balance for what I need.”
– Mike T.
From Total Skeptic to Success: How Cannabis Helped My Skin Condition
“I came to CED Clinic on the recommendation of my dermatologist after battling severe eczema for most of my life. I’d tried everything from steroid creams to light therapy, but nothing seemed to keep the flare-ups at bay for long. The idea of using cannabis for my skin condition seemed strange at first, and I was pretty skeptical. It wasn’t something my friends or family had ever talked about, and I wasn’t sure how it could really help. But my dermatologist convinced me to at least have a conversation, and I’m so glad I did. Dr. Caplan didn’t make me feel awkward or silly for being uncertain. Instead, he walked me through how cannabis could potentially reduce inflammation and improve my skin health. A few months into the treatment plan, and my skin has never looked better. I wish I had come to him sooner.”
– Lindsey P.
Cannabis Helped Me Feel Less Alone
“I’ve been dealing with loneliness for years. After my kids moved out and my spouse passed away, the days just felt so empty. I tried therapy and even medication, but nothing really touched the feeling of being alone. A friend mentioned Dr. Caplan and how cannabis had helped her with anxiety, but I wasn’t sure if it could help with loneliness. It felt strange to think about cannabis as an option for something like that. Still, I figured it was worth a shot. Dr. Caplan was kind and understanding right from the start. He didn’t make me feel silly for bringing up something as hard to explain as loneliness. He explained how cannabis might help ease the constant heaviness I was feeling, not by curing loneliness but by helping me feel more connected to myself and the world around me. We started slow, and over time, I noticed a shift. The emptiness didn’t go away, but it didn’t feel so overwhelming anymore. I started going out more, seeing friends again, and just feeling a little lighter. I’m still working through it, but cannabis—along with Dr. Caplan’s care—has made it easier to handle.”
– Susan R.
Overcoming Arthritis Pain: My Journey to Relief at CED Clinic
“I was referred to Dr. Caplan by my podiatrist, who suggested I look into cannabis after dealing with arthritis in my feet for years. Honestly, I was hesitant. I’d never been a fan of the idea of using cannabis—it seemed like a last resort. But after cycling through endless medications with little success, I was willing to try something new. From the first consultation, Dr. Caplan made me feel completely at ease. He spent time learning about my history and concerns, and he carefully explained the options in a way that was easy to understand. He wasn’t just throwing solutions at me—he was building a plan around my life. I’ve been on the regimen we discussed for about four months now, and the improvement is undeniable. It’s not just the relief, but the care and commitment Dr. Caplan shows that keeps me confident in the process.”
– Robert H.
I Overcame Insomnia with Dr. Caplan’s Help.
“I was referred to Dr. Caplan by my PCP after months of struggling with severe insomnia. For years, I had relied on prescription sleep aids, but over time, they stopped working, and the side effects were unbearable. I had heard about cannabis being used for sleep, but I wasn’t convinced it would work for me. The idea of using cannabis made me nervous—I had no experience with it and didn’t want to feel ‘high.’ But my doctor insisted that I give Dr. Caplan a try, so I booked an appointment. From the very first meeting, Dr. Caplan took the time to understand my fears and hesitations. He didn’t push anything on me but explained how cannabis, especially CBD, could help regulate my sleep cycle without the psychoactive effects I was worried about. His calm, knowledgeable approach reassured me, and we crafted a plan that I felt comfortable with. After just a few weeks on the treatment, I started sleeping better than I had in years. It wasn’t an overnight solution, but Dr. Caplan was with me every step of the way, adjusting the plan as needed. I’ve regained the energy I thought I had lost forever, and for that, I’m incredibly grateful.”
– Rachel S.
Finding Hope After Chronic Migraines: Dr. Caplan Helped Me See Cannabis
“I found Dr. Caplan after reading The Doctor-Approved Cannabis Handbook. I had been suffering from chronic migraines for years, but the idea of using cannabis never crossed my mind. To be honest, I had a lot of doubts—would it work? Would it make me feel ‘off’? But the book opened my eyes to the science behind it, and I decided it was time to explore other options. When I reached out to Dr. Caplan, I was still on the fence, but he took the time to listen, explain, and answer every question I had. He didn’t push anything on me, but instead guided me through the possibilities. Fast forward six months, and I’ve seen such a huge improvement in my quality of life. Dr. Caplan’s approach is professional, but also deeply personal. It’s clear he cares about getting things right for each patient.”
– Jessica M.
No More Painful Periods
“I’ve had awful period cramps for as long as I can remember, and nothing ever worked to ease the pain. My gynecologist suggested Dr. Caplan, but I wasn’t sure about using cannabis for menstrual pain—it seemed kind of odd to me. Still, I was tired of being in pain every month, so I decided to at least talk to him. Dr. Caplan was great—he explained how cannabis could help with cramps and inflammation and answered all my questions without making me feel rushed. He worked with me to figure out a plan that I was comfortable with, and within a few cycles, I started noticing a big difference. The pain isn’t completely gone, but it’s so much more manageable now. I don’t dread that time of the month anymore. I’m so glad I gave it a try—Dr. Caplan’s made this whole process easier than I expected.”
– Emily K.
Trustworthy & Easy
From the moment I first connected with Dr. Caplan on a telemedicine visit, I felt an immediate sense of relief. I had been struggling with anxiety for years, and previous doctors had only offered quick fixes that never addressed the root of the problem. Dr. Caplan took the time to understand my history, my triggers, and my lifestyle. The discussion was open and flowed easily and to me, clearly shows that he actually cares. During our consultation, he explained the complex medical stuff in a way that made sense to me, and made sure I felt informed and empowered every step of the way. When I had a panic attack late one night, I emailed him in desperation, and to my surprise, he responded almost immediately with calming words and practical advice. His personalized follow-up call the next day was the reassurance I needed to stay on track. Dr. Caplan’s unwavering commitment and compassionate care have truly transformed my life.
— Michael Anderson
My anxiety is manageable!
Dr. Caplan’s thoughtful approach turned my anxiety into a manageable journey, offering not just treatment but a renewed sense of hope and understanding.
– S Christianson
I’m a whole person. And I’m complicated.
“I found Dr Caplan after reading his book, The Doctor-Approved Cannabis Handbook. Dr. Caplan doesn’t just treat symptoms—he treats the whole person. From my very first appointment, he made sure I understood every part of my treatment plan, and I left feeling hopeful for the first time in years. His book has been a helpful resource, but it’s his personal touch and thoughtful care that really sets him apart. I’ve never felt rushed or like just another patient in a long line. Instead, I feel truly heard.”
– Sarah W.
My Son Was Right About Cannabis
“Funny enough, my teenage son was the one who pushed me to see Dr. Caplan. I’ve had a stressful job for years, and it’s been taking a toll on my health. My son did a project on cannabis for school and said I should check it out for stress. I was pretty hesitant—I mean, cannabis? It wasn’t something I ever thought I’d try. But after hearing my son talk about it for weeks, I figured, why not? I went to Dr. Caplan with a lot of questions, and he took the time to answer every one of them. He explained how I didn’t have to get ‘high’ to use cannabis for stress and that it could help me feel calmer without messing with my head. He started me on a low-dose CBD plan, and within a couple of weeks, I started noticing a difference. I was less anxious at work, more patient with my family, and just felt more balanced. Honestly, I owe my son for nudging me, but I’m grateful to Dr. Caplan for helping me find a solution that really works.”
– Janet W.
From Sleepless Nights to Peaceful Mornings
“I was dealing with sleepless nights for months—maybe even years—when my primary care doctor suggested I check out Dr. Caplan. I’d been on sleeping pills for ages, but they stopped working, and I was left exhausted all the time. The idea of using cannabis for sleep honestly sounded weird to me. I didn’t know much about it, and I figured it would just make me feel groggy or out of it. But I was tired of being tired, so I made the appointment. Dr. Caplan really gets it—he wasn’t pushy at all. He explained how CBD could help me without the ‘high’ I was worried about, and he was super patient with all my questions. Within a couple of weeks, I was actually sleeping through the night. It’s not an overnight fix, but it’s the best sleep I’ve had in years. I wake up feeling refreshed instead of like a zombie. Dr. Caplan’s follow-ups have been a game-changer too—he checks in to make sure everything’s working. It feels good to have a doctor who cares.”
– Laura B.
Genuine care and great medical advice
Dr. Caplan’s genuine care and commitment are evident in every interaction. At CED Clinic, I received more than just medical advice; I gained a trusted advisor in my health journey. His use of personalized treatment plans and educational resources helped me understand and manage my condition better than ever before.
– Michael T.
Awesome experience!
I never felt like just another patient at CED Clinic; Dr. Caplan made sure of that. His thorough understanding of my health needs, paired with his deep knowledge of cannabis therapy, provided a tailored experience that truly catered to my well-being. Every visit felt like a step forward in my journey dealing with sleeplessness, stress, and PTSD.
– Denise H.
Happy customer!
My visit to CED Clinic was absolutely amazing, and it all started with Kim. She was so friendly and helpful right from the get-go, making the whole scheduling thing a breeze – a real breath of fresh air! Then there was Dr. Caplan. Honestly, chatting with him felt more like catching up with an old friend than a typical doctor’s visit. He didn’t seem to be watching the clock at all; he was all in, really getting to grips with what I’ve been going through, and dishing out advice that hit the nail on the head. And get this – he’s even written a book about it all! I can’t wait to get my hands on a copy. The whole experience at CED Clinic was just so warm and genuine. They’ve got something special going on over there, for sure.
I’m Free: My Journey Beyond Chronic Pain!
I felt trapped in a cycle of chronic pain, where prescription and over-the-counter meds were just dead ends. Then I found Dr. Caplan. His blend of medical expertise and cannabis knowledge opened a door I didn’t know existed. I read ‘The Doctor-Approved Cannabis Handbook’ and it was/is a turning point—packed with research and actionable advice, it guided me to a pain management plan that actually worked. Thanks to Dr. Caplan, I’m living with less pain and more hope. Highly recommend for anyone stuck in the pain cycle.
From Frayed Edges to Balance: Found My Center with Cannabis
Let me paint you a picture of my life not too long ago: a job that never hit ‘pause,’ kids that always needed me in a hundred different ways, and a level of work stress that had me teetering on the edge. I was juggling more plates than I had hands for, and it felt like I was one strong breeze away from watching them all come crashing down. Sleep was a luxury I couldn’t afford, and ‘me time’ was a concept so foreign it might as well have been from another planet.
Enter Dr. Benjamin Caplan and his life-altering approach to managing stress through cannabis medicine. At first, I was skeptical—could this really be the answer I’d been searching for? But from the moment we began, it was clear Dr. Caplan wasn’t just any doctor. His blend of traditional medical insight and innovative cannabis expertise was like a breath of fresh air.
What truly transformed my journey, though, was diving into ‘The Doctor-Approved Cannabis Handbook.’ This wasn’t just another self-help book; it was a treasure trove of evidence-based research, clinical wisdom, and, most importantly, actionable advice that felt like it was written just for me. It became my North Star, guiding me through the haze of stress and sleepless nights to a place of understanding and balance.
Thanks to the personalized strategy Dr. Caplan crafted with me, I’ve been able to reclaim control over my stress and find a sense of equilibrium I didn’t think was possible. My work no longer feels like a constant battle, and I’ve found more joy and presence in the time I spend with my kids. The difference is night and day.
I’m beyond grateful to Dr. Caplan and the invaluable lessons from his handbook. For anyone feeling overwhelmed by the demands of work, family, and everything in between, Dr. Caplan’s compassionate, evidence-based approach might just be the lifeline you need. I can’t recommend him enough.
My Journey to Conquering Chronic Insomnia with Dr. Caplan and Cannabis Medicine
I’ve been in this battle with chronic insomnia for what feels like forever. I hit a point where I felt completely out of options. I mean, you name it, I tried it—all those over-the-counter fixes, prescriptions from my doctors, and I even got creative mixing up my own cannabinoid solutions. But nothing worked. Those endless nights of tossing and turning weren’t just annoying; they were wrecking my health and my spirits.
Then, almost out of nowhere, I stumbled upon Dr. Benjamin Caplan and his work in the world of cannabis medicine. From the moment we started talking, I knew this was different. He’s got this unique blend of traditional medical wisdom and cutting-edge cannabis knowledge. It’s like he sees the whole picture in a way no one else had shown me before.
But here’s the real game-changer: “The Doctor-Approved Cannabis Handbook.” That book blew my mind. It’s packed with solid science and real-deal clinical insights on how cannabis can tackle not just insomnia but a whole list of issues. More than that, it gave me straightforward, practical steps tailored just for me. It turned into my guide on this journey to use cannabis safely and super effectively.
I owe so much to Dr. Caplan and the wisdom packed into that book. I’ve finally found some peace from my insomnia—a relief I thought was off the table for me. My sleep’s way better, and my days? They’ve transformed. I can’t thank Dr. Caplan enough. And seriously, if you’re hitting a wall with insomnia or any health problem that just won’t budge with the usual treatments, Dr. Caplan’s approach could be the breakthrough you’re looking for. Certainly was for me.
Hashimoto’s Disease and Cannabis: How I Found the Right Balance with Dr. Caplan’s Help
“My endocrinologist recommended Dr. Caplan after I’d been diagnosed with Hashimoto’s disease. I was dealing with a range of symptoms—fatigue, joint pain, brain fog—but I was really hesitant to try cannabis. I didn’t have any experience with it and was worried about how it might affect me. Still, after years of feeling like nothing was really working, I was ready to explore new options. Dr. Caplan’s approach made all the difference. He took the time to understand not only my medical history but also my reservations. He patiently explained how cannabis could help with my symptoms without overwhelming me. It wasn’t an instant fix, but over the months, I started noticing real improvements. What sets Dr. Caplan apart is how much he truly listens and adapts the treatment plan to my needs. I’ve never felt more supported by a doctor.”
– Megan L.
A Lifeline in Chronic Pain: Cannabis Changed My Life
“I was referred to Dr. Caplan by my orthopedist after years of dealing with debilitating lower back pain. I had been through physical therapy, painkillers, and injections, but nothing offered lasting relief. Honestly, I was skeptical about trying cannabis. I had always associated it with recreational use and didn’t see how it could be a solution for chronic pain. But after my orthopedist explained the potential benefits and encouraged me to meet with Dr. Caplan, I decided to give it a chance. From the moment I walked into Dr. Caplan’s office, I felt like he was different from any doctor I’d seen before. He listened carefully to my history and my concerns, and instead of pushing cannabis on me, he educated me on the science behind it. He explained how it could help reduce inflammation and manage pain without the foggy side effects I was used to with traditional medications. Now, after six months of working with Dr. Caplan, my pain is more manageable than I ever thought possible. I’m not saying it’s a magic cure, but for the first time in years, I feel like I have control over my life again. His compassion and expertise have been a lifeline for me.”
– David P.
Used as a Human Target as a Kid, Medical Cannabis is the answer.
I’m totally blind. I live in a rural area. So when I was 12, same-age peers thought zapping the blind girl’s eyes with laser pointers would be a great idea. It got bad enough that my paraprofessional had to have the devices banned from the school for my safety. Shortly after, I began having intense eye aches. I differentiate them from headaches because even a 12 year old can tell the difference. Doctors told my parents and I they were migraines. It wasn’t until later in life that I began realizing there was something else going on here. Really studying migraines, studying the eye, studying neurology and understanding not all was as it seemed. I began developing my own theories as to what these “migraines” were. I take migraine meds, but they don’t treat the eye aches. They treat the other migraine symptoms just fine. My younger brother suggested I try edibles last year. Because by this point, I was in enough pain where I believed I’d have to have my eyes removed. None of us wanted to see that happen. So he took me to a dispensary, (he had spoken with someone he knew there about me prior, and they’d come up with a regimen they thought would work.) The first clue I had that we were on the right track, was that I slept for 14 hours. So I kept a calendar and a spreadsheet full of virtual sticky notes, and 2 weeks later came to Dr. Caplan for my medical card, crazy theories about optic neuropathy in underdeveloped optic nerves and all. A year later, I’m studying cybersecurity, because that’s something I found I’m passionate about, and I can do it now!
To sleep well again is life-changing
Dr. Caplan was coincidentally recommended by both my dentist and a close friend. I was concerned about finding a high level, knowledgeable, physician in a professional setting who understood using cannabis in a safe and effective manner. I can’t recommend Dr. Caplan more highly. His knowledge is vast and I am grateful for his expertise, care and compassion. To sleep well again is life-changing. Very few things literally change someone’s life. Dr. Caplan’s knowledge and guidance on cannabis did that for me.
Not once did I feel rushed or embarrassed, in fact I felt like he really does care about my circumstances, and wanted for me to feel confident and prepared
Honestly, I was hesitant to try cannabis. I have debilitating menstrual cramps and my OB/GYN recommended Dr. Caplan. I was more than a little hesitant to try cannibas because all I really knew about it was that people used it to get “high” – and that was not something I was interested in. This perspective totally changed when I actually came in and met with Dr. Caplan. He was incredibly understanding and really took the time to ease my mind about the whole process, what kind of options there were to choose from, what they might do, and what would probably appeal to me. He spent a lot of time answering all my questions (and I had a lot!). Not once did I feel rushed or embarrassed, in fact I felt like he really does care about my circumstances, and wanted for me to feel confident and prepared.
Dr. Caplan was thorough in his evaluation and friendly and accessible in his approach
Dr. Caplan was thorough in his evaluation and friendly and accessible in his approach. He provided in depth information and step by step guidance for beginning the process of utilizing cannabis therapies. He is available to his patients by email and phone. I highly recommend an appointment with him if you are even remotely considering medicinal use. I was hesitant about this approach before my appointment but now, after talking with Dr. Caplan and learning a little bit more about the science, I am eager to explore and I feel better already!
I saw Dr Caplan a few months ago, and from even before I met him, he has made himself available to me over email, for questions, more than even my regular doctor
I came into marijuana medicine with zero experience. I must say, I’ve been learning a ton, and I would recommend it to anyone with terrible anxiety and depression. I saw Dr Caplan a few months ago, and from even before I met him, he has made himself available to me over email, for questions, more than even my regular doctor. A friend told me that I should see Dr Caplan, but I was still unsure about becoming a medical marijuana patient. I called and was able to speak with Dr Caplan directly. He took time, on the phone, even before he had met me, to explain the whole process, which helped me feel more comfortable putting a voice and personality to the process. Later, when I finally came in, during the visit, he spent almost 40 minutes with me, walking me through how cannabis might fit in with some of the other treatments I currently use. We have kept in touch over email since, like 3 or 4 random questions, and has always responded promptly. I think he is a truly special doctor, and from what I’ve read on Twitter, has a passion for educating and helping improve the perception of cannabis.
I had an enjoyable visit with clear information and education about medical marijuana and the dispensaries
Full stars. I appreciate the great parking and simple scheduling system. I had an enjoyable visit with clear information and education about medical marijuana and the dispensaries. No fancy language, no time wasted. Works for me.
I am a survivor of breast, uterine, and ovarian cancers, and Dr Caplan of CED Clinic is, hands down, the favorite voice of support and cannabis education for our hospital list-serv care group
I am a survivor of breast, uterine, and ovarian cancers, and Dr Caplan of CED Clinic is, hands down, the favorite voice of support and cannabis education for our hospital list-serv care group. I have seen him speak publicly, and on TV, and of course he is also my doctor. In spite of having what seems to be a crowd of patients who are mostly in terrible pain or have a generous helping of emotional/mental issues, I see him work tirelessly for his patients and for the cause, in general. I appreciate his leadership in the cannabis field. He is one in a million.
Dr. Caplan is an extremely knowledgeable doctor in his field and very easy to speak with about any questions and concerns you may have
Dr. Caplan is an extremely knowledgeable doctor in his field and very easy to speak with about any questions and concerns you may have. As a person that suffers from anxiety, upon arriving at the office I felt welcomed and relaxed because the doctor is compassionate and kind. The office atmosphere is not what I expected at all and was very peaceful and relaxing, also there were snacks and beverages which I have never seen before in a doctor’s office. I would highly recommend Dr. Caplan because he will take the time to answer every question that you may have about treatment. I made an appointment on a Saturday and was seen right away on the same day! Very easy process and very responsive. I am happy I chose Dr. Caplan!
This is our second visit to Dr. Caplan in a year, and on both occasions, we were just blown away by his caring and compassion
This is our second visit to Dr. Caplan in a year, and on both occasions, we were just blown away by his caring and compassion. He is a true healer, with a great heart, enormous patience, and extraordinary expertise. My wife and I were amazed to find a physician who truly puts his patients first, and who is passionate about figuring out the best way to help us with our chronic pain. In our 60+ years of experience with health care providers, Dr. Caplan is among the most committed, generous, and caring healers we have ever met.
I can’t recommend Dr. Caplan highly enough
I can’t recommend Dr. Caplan highly enough. This was my third medical marijuana certification review (original plus two renewals), and the previous two doctors were just perfunctory form-fillers in shabby offices in remote office parks. Dr. Caplan is a REAL cannabis doctor who’s deeply knowledgeable about medical marijuana and clearly explains EXACTLY how to use it for YOUR specific conditions. He also has a real doctor’s office in a real medical building right on Boylston Street (Route 9) in Chestnut Hill ( not far from NETA Brookline, my dispensary of choice.) AND THE VISIT IS COVERED BY MEDICAL INSURANCE! I’ve become somewhat knowledgeable about what works for my primary complaint (chronic pain from spinal stenosis w/ radiculopathy) and what to avoid, but he gave me brand new ways to deal with my insomnia (including how and when to use edibles, which hadn’t worked for me before b/c I didn’t really know what I was doing) and arthritis in my hands (including a simple recipe to make topical lotion that’s stronger and cheaper than the commercial products). I interrupted him with frequent questions, which he answered at whatever level of detail and technical information I wanted. I had been deeply dissatisfied with the cannabis doctors I went to before, but Dr. Caplan is an outstanding DOCTOR who happens to specialize in medical marijuana because he cares about helping patients for whom traditional medicine hasn’t fully met their needs. You can book appointments on his web site, although my wait time was more than 10 minutes (during which I filled out his online patient questionnaire on my phone and ate all the Kit Kats in his candy basket), it was well worth it. This is a relatively new practice, I believe, and it’s going to get a lot busier as word spreads. But just do yourself a favor and go: this is what state-of-the-art medical marijuana care is supposed to be like.
Dr. Caplan patiently explained how there are so many options to chose from and exactly what each was helpful for
I recently had my first appointment with Dr. Caplan after reading negative reviews of so many other medical marijuana certification “places”. I can’t say enough good things about my visit with him. To start with he’s a very compassionate, caring doctor. I’m a 63 yr old woman and had never used marijuana or “street drugs”, so I was feeling nervous about trying it. I recently started chemo therapy at Dana-Farber and the side effects have been difficult to deal with. In particular, insomnia and a bit of evening anxiety. He is extremely knowledgeable about all aspects of medical marijuana. Dr. Caplan patiently explained how there are so many options to chose from and exactly what each was helpful for. With that said, he suggested several products for me to try. I now know what helps me, but each person has to use the information he gives and then try different products from a reputable medical dispensary. I plan to have a 2nd appt. with him in a few months just to get his feedback on my experiences and possibly more recommendations. It’s not necessary to go back to him after getting your certification, but he truly knows so much about the medicinal benefits that I’d like to learn even more. I highly recommend him.
I would highly recommend Dr. Caplan because he will take the time to answer every question that you may have about treatment
Dr. Caplan is an extremely knowledgeable doctor in his field and very easy to speak with about any questions and concerns you may have. As a person that suffers from anxiety, upon arriving at the office I felt welcomed and relaxed because the doctor is compassionate and kind. The office atmosphere is not what I expected at all and was very peaceful and relaxing, also there were snacks and beverages which I have never seen before in a doctor’s office. I would highly recommend Dr. Caplan because he will take the time to answer every question that you may have about treatment. I made an appointment on a Saturday and was seen right away on the same day! Very easy process and very responsive. I am happy I chose Dr. Caplan!
Dr. Caplan is extremely patient and compassionate
Dr. Caplan is extremely patient and compassionate. He answered all of my questions and gave me a great deal of useful information (while emphasizing that I didn’t have to absorb all of it right away). He encouraged me to contact him with any more questions I might have after the appointment, and began the process of registering me immediately after I left. I had an email from the Commonwealth of MA before I got home, and completed the application online within a few minutes. It couldn’t have been an easier or more stress-free experience. Dr. Caplan truly believes in the effectiveness of cannabis as a medicinal tool, and is committed to making it more widely available for that purpose and in dispelling the ocean of ignorance that has unfortunately been created around it in our society. I can’t recommend him highly enough.
Excellent Experience, top to bottom
Excellent Experience, top to bottom. I scheduled my appointment on CED clinic website, got in the next day – and visit was informative, and doc was kind, compassionate, and amazingly knowledgeable. I intend to follow him as a permanent addition to my healthcare and would recommend widely.
I’m shy but felt comfortable and supported
Awesome doctor. Super easy to talk to. I’m shy but felt comfortable and supported. Great teacher too. I had no idea there was so much to know!
I learned about different options and lots of choices, and received handouts to learn even more
First heard of Dr Caplan on /r/BostonTrees subreddit. Made my appointment online, for the next day, and did all paperwork online before I came in. Building is very professional and comfortable, with great parking, and close to where I live. As I expected, doc was kind, thorough, and efficient. We reviewed my medical history, talked about what I had been doing in the past, and discussed a host of treatment ideas, and not just marijuana. I learned about different options and lots of choices, and received handouts to learn even more. I plan to follow up in a few months, and I look forward to it.
Every time I come in, I learn something new and amazing.
I followed Dr Caplan from his position as the Medical Director of Canna Care Docs to CED Clinic – and would follow him again. I have had years of back pain and arthritis – my wrists and knees and hips. Dr Caplan has helped me understand much more about marijuana, and I have to say, it has been a wonderful improvement for me. Every time I come in, I learn something new and amazing. It’s a new industry for me, and I feel very well supported.
My visit with Dr. Caplan made it comforting to know that someone was on my side
My visit with Dr. Caplan made it comforting to know that someone was on my side. I was surprised to find that Dr. Caplan does more than just write scripts for people to take to dispensaries. He sees some of his patients on a regular basis to personalize treatment plans and it’s clear he cares about education and the destigmatization of medical cannabinoids. He goes to assisted living centers, medical expos, wellness centers, and more to speak with people on the matter. This is his passion!
Dr. Caplan is extremely patient and compassionate
Dr. Caplan is extremely patient and compassionate. He answered all of my questions and gave me a great deal of useful information (while emphasizing that I didnâ€t have to absorb all of it right away). He encouraged me to contact him with any more questions I might have after the appointment, and began the process of registering me immediately after I left. I had an email from the Commonwealth of MA before I got home, and completed the application online within a few minutes. It couldn’t have been an easier or more stress-free experience.†“— Dr. Caplan truly believes in the effectiveness of cannabis as a medicinal tool, and is committed to making it more widely available for that purpose and in dispelling the ocean of ignorance that has unfortunately been created around it in our society. I can€t recommend him highly enough.
Very knowledgeable and compassionate
Very knowledgeable and compassionate.
I would highly recommend Dr. Caplan
I wasn’t sure what to expect from the initial appointment. It was informative, educational and an overall great experience! Dr. Caplan is easy-going, kind, and gave clear, detailed information about medical cannabis and MA medical dispensaries. I would highly recommend Dr. Caplan. His clinic and his knowledge are certainly worth 5-star reviews!
I had such a good experience with Dr. Caplan of CED Clinic.
I had such a good experience with Dr. Caplan of CED Clinic.
Medical: I had a lot of worries going in, and Dr. Caplan put me at ease with his knowledge and calm manner. As a family doctor, he asked good questions about my extensive medical background, in a supportive way. He used normal people words instead of medical gobbledygook! (I had just an hour before been at an appointment with a medical person who thought I should understand when he talked about my distal iliolumbar neuropathy – or something like that, I had no idea what he was talking about – so I especially noticed when Dr. Caplan used normal words that any person would know.)
Educational: He provided excellent information for total newbies, showed some devices, talked about legal stuff, and gave great info about local clinics and huge discounts available. I’m used to doctors providing pretty poor education materials, but Dr. Caplan’s infographics and handouts were a thing of beauty – informative, easy to read, and visually simple. I hope Dr. Caplan writes a book because I will buy it.
Logistics: This is such a streamlined practice, it is easy to get in soon, and respectful of your time. I got an appointment within less than 2 days, scheduled online, filled out my info online beforehand, found parking easily, was in and out quickly, and received the email with next steps instructions and application activation code in 1.5 hour! Can’t possibly be easier than this.
Dr. Caplan was very friendly, extremely helpful and knowledgeable
Dr. Caplan was very friendly, extremely helpful and knowledgeable. I would definitely recommend and I am looking forward to having him as a health resource.
I’ve switched 100% to cannabis as my go-to medicine
I’ve switched 100% to cannabis as my go-to medicine. I’m sick of pharmaceuticals; the weight gain, the weird feelings like I’m a zombie, the miserable sleep…sorry, but hard pass. Weed helps take the edge off and I’m still fully functional.
Dr Caplan's Book: The Doctor-Approved Cannabis Handbook
"A wealth of information and a huge dose of compassion and clarity."
- Melissa Etheridge
Get To Know Your Medical Team!
We Stay Connected With Our Patients via Email, Online, and Even on the Airwaves!
Email | Instagram | Twitter | LinkedIn | YouTube | Spotify | Newsletter
CaplanCannabis.com | The Commonwealth Project | EO Care | Green Table Talk Podcast

😎
Sounds too good to be true? Put us to the test!
Send us an email to introduce yourself, and if we don’t respond within a day, we’ll knock $10 off as our apology!
SAVE Money 💰 with CED Clinic:
Your health shouldn’t break the bank—let us help you save!
Contact us here for more
The Latest




































 Study highlights pros, cons of medical marijuana as its future in Tennessee remains unknown" class="wplp_thumb" />
Study highlights pros, cons of medical marijuana as its future in Tennessee remains unknown" class="wplp_thumb" /> Study reveals cannabis compounds reduce threat of fatty liver disease | Health – WFMZ.com" class="wplp_thumb" />
Study reveals cannabis compounds reduce threat of fatty liver disease | Health – WFMZ.com" class="wplp_thumb" /> Study reveals cannabis compounds reduce threat of fatty liver disease | Health – News-Topic" class="wplp_thumb" />
Study reveals cannabis compounds reduce threat of fatty liver disease | Health – News-Topic" class="wplp_thumb" />