A calm, evidence-based unpacking of what the latest MASH cirrhosis data actually shows, and what it doesn’t
This post walks through what the “Cannabis Use Disorder Heart Attack Study” actually measured, what it could plausibly mean, and which conclusions it does not support.
This is educational content, not individualized medical advice. If you have MASH cirrhosis or cardiovascular disease, decisions should be personalized with your care team.
TL;DR
The point in five lines- 🧾The Cannabis Use Disorder Heart Attack Study found higher odds of heart attack in hospitalized MASH cirrhosis patients labeled with CUD.
- 🏷️The study measured a diagnosis code, not dose, route, timing, or biological exposure.
- 📊Cross-sectional hospital data cannot prove causation.
- 🧠CUD is a behavioral-psychiatric construct, not a precise pharmacologic variable.
- 🧭This study raises important questions, but it does not justify panic or simplistic conclusions.
What You’ll Learn in This Post
- 🔍What the study actually measured:
What “exposure” meant in this dataset, and what it did not mean. - ⚖️ICD-coded CUD vs quantified THC exposure:
Why “use disorder” is not a dose-response variable. - 🫀Why liver disease complicates cardiovascular interpretation:
Demand ischemia, hemodynamic stress, and background risk. - 🧩Where confounding and coding bias can shape results:
Documentation intensity, comorbidity clustering, and social context. - 🗣️What thoughtful clinicians can say today:
How to speak with patients without stigma, fear, or false reassurance.
The Cannabis Use Disorder Heart Attack Study: What It Claimed and Why It Matters
A new Cannabis Use Disorder Heart Attack Study examined hospital data from adults with metabolic dysfunction-associated steatohepatitis, or MASH cirrhosis. The headline finding sounds striking: patients diagnosed with cannabis use disorder had roughly double the odds of experiencing an acute myocardial infarction during hospitalization.
When you see the words “heart attack” and “cannabis” in the same sentence, attention spikes. It should. Cardiovascular disease is not trivial. Nor is MASH cirrhosis, a serious liver condition tightly linked to metabolic disease, diabetes, and obesity.
Key idea: Before a headline hardens into dogma, we need to ask one boring, essential question: what exactly was measured?
Because in science, the measurement is everything. In this case, the measurement was not cannabis exposure. It was a diagnosis code.
Study: Cannabis Use Disorder Is Associated With Increased Risk of Acute Myocardial Infarction in Adults With Metabolic Dysfunction-Associated Steatohepatitis (MASH) Cirrhosis: A Population-Based Analysis
Authors: Basile Njei, Sarpong Boateng, Ifeoma Kwentoh, Prince Ameyaw, Chukwunonso Ezeani, Nso Nso, Sabastian Forsah, Christian A. Dimala, Derek Fan Ugwuedum, Lea-Pearl Njei, Yazan A. Al-Ajlouni, Joseph K. Lim, Jonathan A. Dranoff
DOI: 10.7759/cureus.103299
What the Study Actually Did (Without the Drama)
The researchers used a large national inpatient database. That means they analyzed hospital discharge records, not outpatient visits, not prospective tracking, and not controlled trials.
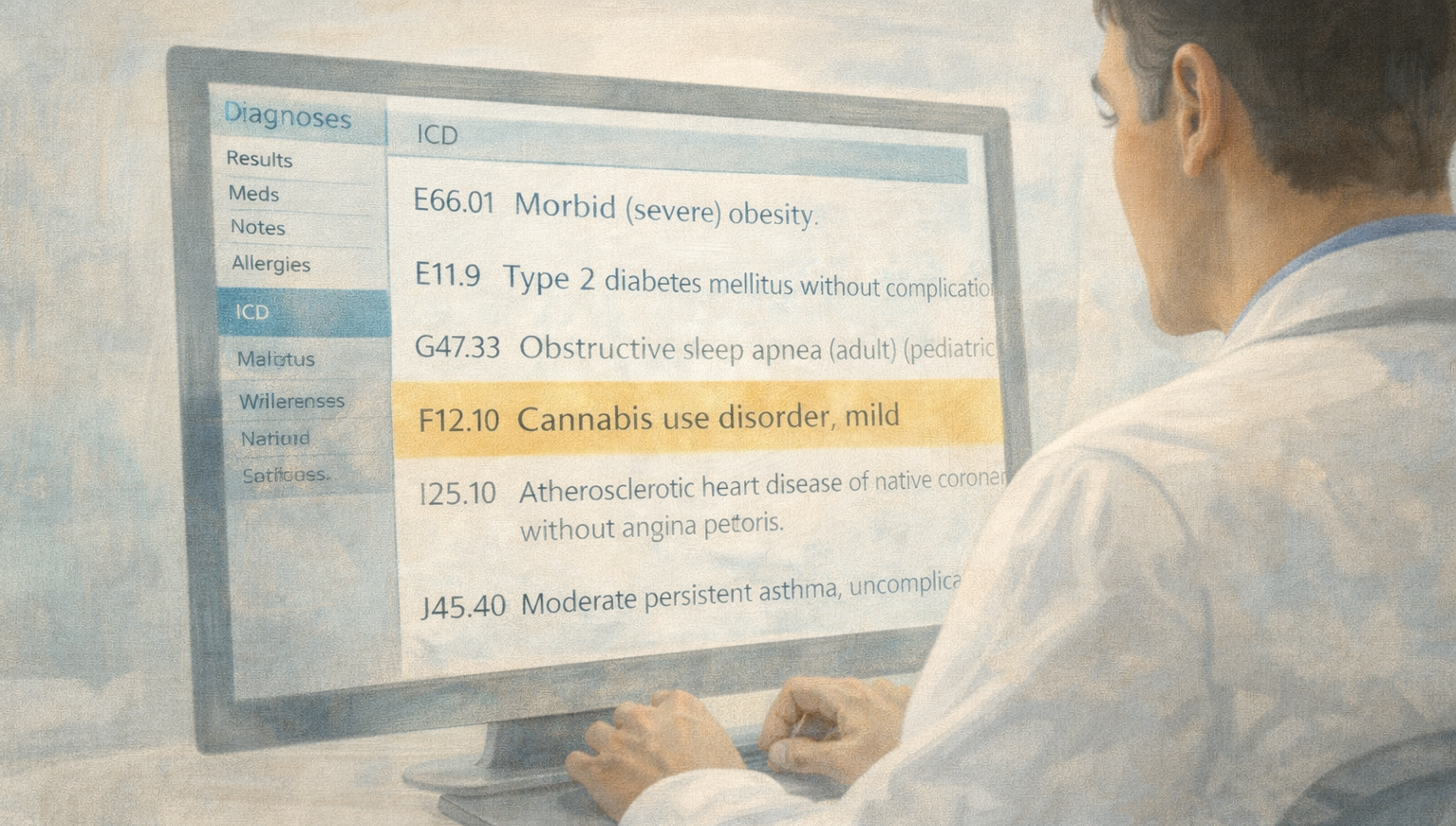
They identified patients hospitalized with MASH cirrhosis, then separated them into two groups: those with an ICD-coded diagnosis of Cannabis Use Disorder, and those without that diagnosis.
An ICD code is a documentation and billing label.
It reflects what clinicians recorded and what coders entered. It does not measure THC dose, frequency of use, route of administration, timing of last use, blood cannabinoid levels, or severity of intoxication.
The study then asked: during these hospitalizations, were heart attacks more common among those labeled with cannabis use disorder? Statistically, the answer in this dataset was yes.
But this is where the interpretation becomes more nuanced, and also more clinically useful.

The Entire Study Hinges on a Label
The exposure variable was not cannabis pharmacology. It was a psychiatric diagnosis: Cannabis Use Disorder, or CUD.
This distinction is not pedantic, it is foundational.
CUD is defined behaviorally in the DSM-5. It blends biology, psychology, context, and clinician interpretation. That makes it meaningful, but not pharmacologically precise.
CUD criteria include elements like using more than intended, difficulty cutting down, time spent obtaining or using, craving, tolerance, withdrawal, social impairment, and hazardous use.
- 🧬Tolerance is biology.
- 🧠Craving is psychology.
- 🏥Coding is sociology.
Severe, functionally impairing CUD absolutely exists. The issue is that this dataset cannot tell you whether the elevated risk signal is driven by severe cases, mild cases, or a mixed group. It also cannot tell you what, specifically, the cannabis exposure looked like.
Why MASH Cirrhosis Complicates Everything
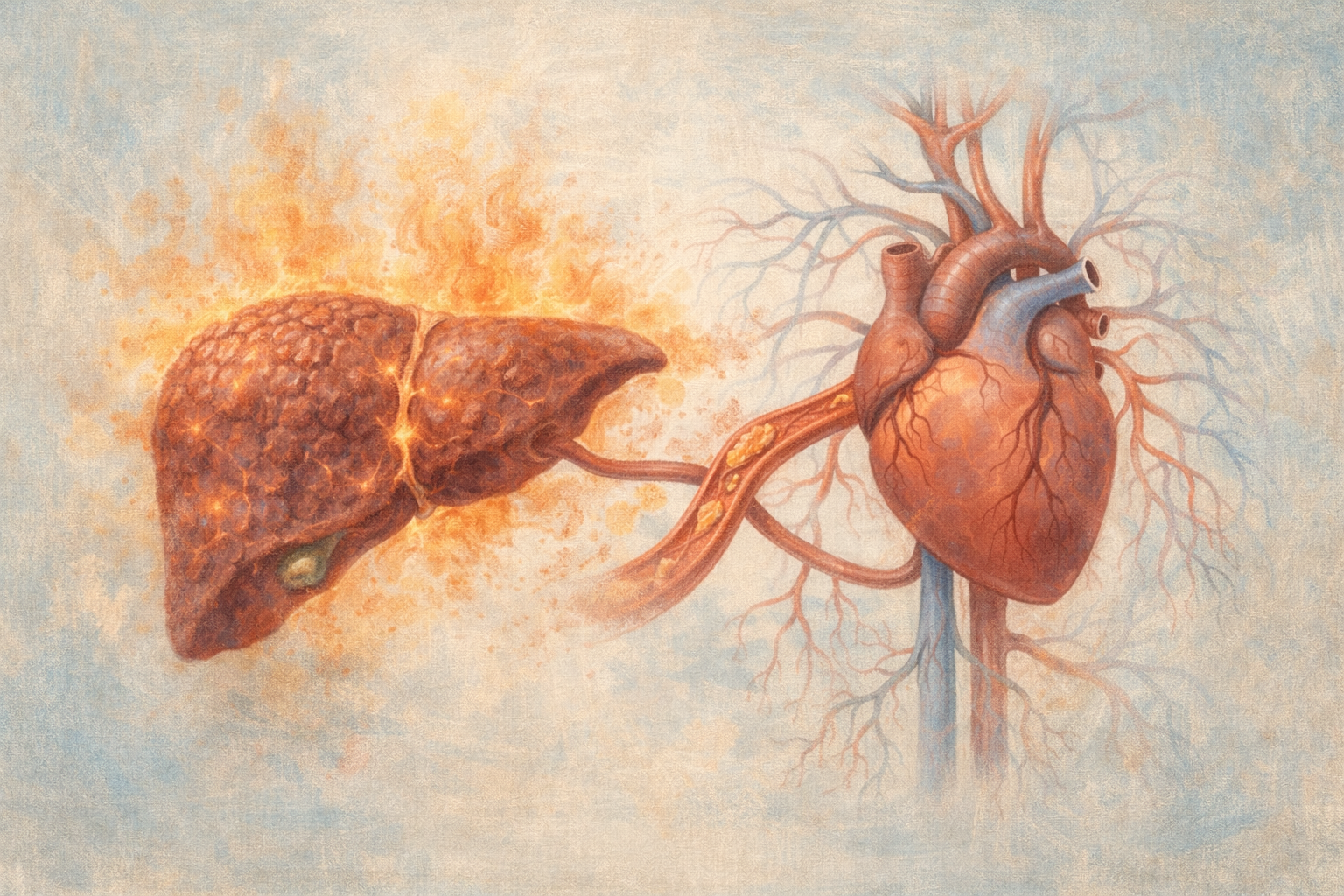
MASH cirrhosis is not a neutral backdrop. It is a high-risk metabolic environment. Patients often have insulin resistance, hypertension, dyslipidemia, chronic inflammation, and endothelial dysfunction, each of which can independently increase cardiovascular risk.
More on metabolic conditions and cannabis (context, not conclusions): https://cedclinic.com/metabolic-endocrine-and-energy-disorders/
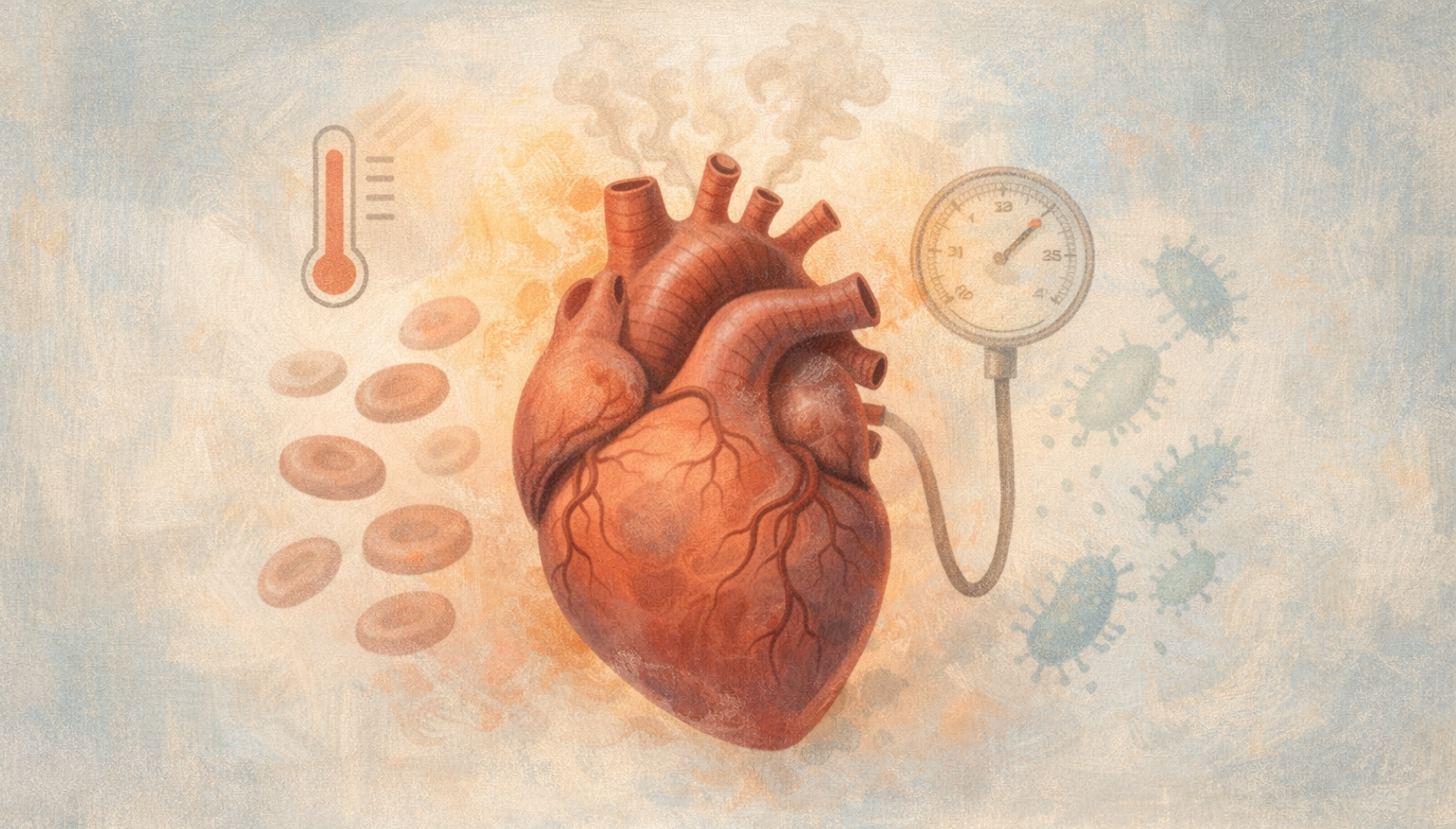
When someone with MASH cirrhosis is hospitalized, physiologic stressors stack up: infection, anemia, fluid shifts, and blood pressure instability. These can contribute to what cardiologists call type 2 myocardial infarction, sometimes described as demand ischemia. That differs from a classic plaque-rupture heart attack.
The key question the dataset cannot answer:
Are we seeing a pharmacologic effect of cannabinoids on coronary biology, or a clustering of vulnerability and stress physiology in patients more likely to be labeled with CUD?
Administrative data usually cannot disentangle those mechanisms cleanly.
The Subtle Power of Coding
Administrative hospital data depends on documentation. Not every cannabis user receives a CUD diagnosis. In fact, most do not.
CUD coding can correlate with socioeconomic factors, polysubstance use, psychiatric comorbidity, payer status, and documentation intensity. In many datasets, it also tracks with urban teaching hospitals.
Reframe: The study may be identifying a risk marker, not isolating a molecular culprit.
A smoke alarm tells you there is smoke. It does not tell you whether it came from a toaster, a wiring fault, or a fireplace.
A Brief Word on Stigma and Diagnostic Elasticity
The diagnosis of Cannabis Use Disorder spans a spectrum from mild to severe. Two criteria over twelve months qualifies as mild CUD, which can include tolerance plus an occasional unsuccessful attempt to cut down. That does not make it meaningless. It does mean the category is broad.
Related reading on dependence framing and myths:
Memorable middle: Tolerance is biology. Craving is psychology. Coding is sociology.
Dog-face, frog-face, bog-face. Once we name something, it starts to behave like the name in public conversation, even when the underlying reality is more complicated.
Alternative Explanations: When Association Is Not Accusation
If you strip the finding down to its statistical core, it says this: among hospitalized patients with MASH cirrhosis, those labeled with CUD had higher odds of a documented myocardial infarction.
That is a valid association within that dataset. It is not a built-in explanation.
- 🚬Polysubstance clustering:
CUD coding may correlate with tobacco use, stimulant exposure, or alcohol misuse, which can meaningfully change cardiovascular risk. - ⚠️Severity bias and stress physiology:
Patients coded with CUD may present with more acute stress states, psychiatric distress, or social instability, all of which can influence in-hospital events. - 🧪Type 2 MI coding blur:
In cirrhosis, anemia and hemodynamic instability are common. Demand ischemia may be coded as MI in administrative records. - 🗂️Documentation intensity:
Some hospitals code substance use disorders more frequently than others. The association may partly reflect charting behavior.
Bottom line: This signal warrants attention, not panic. It calls for better measurement, not louder headlines.
Type 2 Myocardial Infarction and Why It Can Confuse the Outcome
Type 2 myocardial infarction refers to heart muscle injury caused by oxygen supply-demand mismatch rather than a classic blocked artery. Stressors like anemia, infection, sepsis physiology, hypotension, tachyarrhythmias, and hemodynamic instability can contribute.
In patients hospitalized with cirrhosis, these stressors are common. Administrative databases often do not cleanly separate myocardial infarction mechanisms, which can blur interpretation of “heart attack” outcomes in inpatient datasets.

What This Study Does Mean for Patients and Clinicians
Calmly interpreted, this study suggests something clinically reasonable: in hospitalized patients with advanced metabolic liver disease, being labeled with CUD tracks with higher cardiovascular vulnerability.
That means cardiovascular risk assessment matters, and substance-use pattern review matters. If someone with MASH cirrhosis uses cannabis daily, particularly in inhaled form, and especially alongside tobacco or stimulants, that deserves thoughtful discussion, not moral panic, not shame.
Broader cardiovascular context:
If a patient asks, “Did cannabis cause the heart attack?”
An honest answer is: this study cannot prove that. It shows correlation within hospitalized patients using a diagnosis label. It raises important questions. It does not settle them.
Cannabis and Cardiovascular Health: The Larger Evidence Landscape
The relationship between cannabis and cardiovascular health remains complex. Some observational studies suggest increased cardiovascular events among heavier users, others show mixed or non-significant findings. Mechanistically, cannabinoids can influence heart rate, vascular tone, inflammation, and autonomic signaling, but dose, route, tolerance, and co-use change the story.
There is no credible evidence that cannabis is uniformly benign for the cardiovascular system. There is also no definitive evidence that cannabis independently doubles heart attack risk across populations in a clean, causal way.
Precision beats polarization.
We are rarely talking about a binary. We are talking about dose, context, individual biology, route of administration, and co-existing disease.
A Necessary Acknowledgment: Severe Cannabis Use Disorder Is Real
It is important not to swing from stigma to dismissal. Severe CUD exists. There are individuals for whom use becomes compulsive, impairing, destabilizing. Withdrawal cycling can occur. Functional decline can happen.
What administrative datasets cannot do is stratify severity cleanly. Mild and severe diagnoses may occupy the same exposure category in a national inpatient study. That uncertainty should temper conclusions.
So Where Does This Leave Us?
In a surprisingly steady place. This study should not be dismissed. It highlights a cardiovascular signal in a high-risk hospitalized population. It also should not be over-interpreted. It does not prove that cannabis pharmacology independently causes heart attacks in patients with MASH cirrhosis.
For patients, the message is not panic. It is precision.
A practical next step:
If you have metabolic liver disease, cardiovascular risk assessment is critical. If you use cannabis, especially heavily or alongside other substances, bring it into the open with a clinician who can discuss it without stigma.
If you are unsure whether medical cannabis is appropriate for your situation, start here: https://cedclinic.com/how-to-know-if-medical-cannabis-is-right-for-you/
The goal is not to defend a plant. The goal is to defend clarity.
Careful reading. Careful thinking. Careful care.
FAQ
Cannabis Use Disorder, MASH cirrhosis, and myocardial infarction1) What did the Cannabis Use Disorder Heart Attack Study actually find?
The Cannabis Use Disorder Heart Attack Study reported that hospitalized patients with MASH cirrhosis who carried an ICD-coded diagnosis of cannabis use disorder had higher odds of a documented myocardial infarction during that admission. Crucially, the study relied on hospital discharge records rather than direct measurement of cannabis exposure. That means it identifies an association within administrative data, not proof of causation. The difference between correlation and causation is central to interpreting the result.
2) Does cannabis cause heart attacks in patients with liver disease?
This study does not prove that cannabis directly causes heart attacks. It observed an association between an ICD-coded cannabis use disorder diagnosis and myocardial infarction among hospitalized patients with MASH cirrhosis. Because the analysis is cross-sectional and based on administrative coding, it cannot establish temporality, dose-response relationships, or biologic mechanism. Causal claims require stronger prospective and mechanistic evidence.
3) What is MASH cirrhosis and why does it matter for heart health?
MASH cirrhosis refers to advanced metabolic dysfunction-associated steatohepatitis, a severe form of fatty liver disease. Many patients with MASH also have diabetes, obesity, dyslipidemia, hypertension, and systemic inflammation, each of which independently increases cardiovascular risk. In other words, this population starts with elevated heart attack risk before cannabis is considered. That background risk complicates interpretation of additional associations seen in hospital datasets.
4) What is Cannabis Use Disorder and how is it diagnosed?
Cannabis Use Disorder (CUD) is a DSM-5 psychiatric diagnosis based on behavioral criteria such as difficulty cutting down, tolerance, withdrawal, craving, hazardous use, and functional impairment. Clinicians diagnose it and it may be captured in medical records as an ICD code. It does not directly measure THC concentration, product potency, route of administration, frequency, or timing. As a result, CUD is a heterogeneous construct blending biology, behavior, and clinical documentation.
5) What are ICD codes and why do they matter in this study?
ICD codes are standardized diagnostic labels used for medical documentation and billing. In this study, the “cannabis exposure” variable was defined by the presence of an ICD-coded Cannabis Use Disorder diagnosis. ICD coding practices can vary across hospitals, clinicians, and regions, and may reflect documentation intensity as much as biology. That variability introduces important measurement limitations in large database studies.
6) What is type 2 myocardial infarction and could it affect the findings?
Type 2 myocardial infarction refers to myocardial injury caused by oxygen supply-demand mismatch rather than a classic coronary artery blockage from plaque rupture. Stressors such as anemia, infection, sepsis, hypotension, tachyarrhythmias, and hemodynamic instability can contribute. In patients hospitalized with cirrhosis, these stressors are common. Administrative databases often do not clearly distinguish MI subtypes, which can blur interpretation of “heart attack” outcomes in inpatient datasets.
7) Could socioeconomic factors influence the Cannabis Use Disorder Heart Attack Study results?
Yes. The study’s pattern, including higher rates of Medicaid coverage and care in urban teaching hospitals among patients coded with CUD, suggests that socioeconomic gradients and healthcare access patterns may influence both outcomes and coding. Social determinants of health can affect cardiovascular risk and can also shape how substance-related diagnoses are documented. These factors may contribute to the observed association in administrative data.
8) Is Cannabis Use Disorder always severe?
No. Cannabis Use Disorder spans a spectrum from mild to severe. Mild CUD can be diagnosed when as few as two criteria are present over a twelve-month period. Many administrative datasets cannot stratify severity in a clinically meaningful way. As a result, a single “CUD” exposure category may include a heterogeneous population, which complicates interpretation of risk estimates.
9) Should patients with MASH cirrhosis avoid cannabis completely?
There is no universal answer. Patients with advanced liver disease already carry elevated cardiovascular risk and should have individualized discussions about cannabis, including route, dose patterns, co-substance exposures, and the specific symptom goal. Inhaled cannabis combined with tobacco or stimulant use may carry different considerations than carefully dosed oral or sublingual formulations. Shared decision-making with a knowledgeable clinician is the right frame, rather than blanket bans or blanket reassurance.
10) What is the takeaway from the Cannabis Use Disorder Heart Attack Study?
The takeaway is not panic, and not dismissal. The study identifies an association that warrants thoughtful attention in a high-risk metabolic population. It does not establish definitive causation or isolate cannabis pharmacology as the driver. Careful interpretation protects scientific integrity and patient trust, and it helps clinicians translate “headline risk” into practical, individualized guidance.
Fair view: “This study is a signal, not a verdict. It tells us to assess cardiovascular risk and substance use patterns carefully in MASH cirrhosis. It does not tell us that cannabis exposure alone caused a heart attack.”