Table of Contents
- Why the pandemic’s quiet rewiring of daily life is now showing up in bodies, clinics, and aging
- Naming the Post Covid Baseline We’re All Living In
- Public Life Got Strange and No One Knows How to Name It
- Weak Ties Vanished and Health Became Harder to Detect
- Self-Triage Became the New Primary Care
- The Post Covid Baseline Lives in the Nervous System
- Long Covid: The Concentrated Version
- Clinicians Are Living in This Baseline Too
- Older Adults as the Cultural Canary
- Where Cannabis and the ECS Fit in the Post Covid Baseline
- What to Do with a Baseline You Did Not Choose
- FAQS about the new Post-COVID Baseline
- 1. What is the post Covid baseline?
- 2. How does the post Covid baseline affect mental health?
- 3. Why do social interactions feel harder after Covid?
- 4. What are weak ties and why do they matter for health?
- 5. How did Covid change healthcare-seeking behavior?
- 6. What is the relationship between long Covid and the post Covid baseline?
- 7. How does the nervous system play a role in post Covid symptoms?
- 8. Where does cannabis fit into the post Covid baseline?
- 9. Why were seniors affected more by post Covid changes?
- 10. Can the post Covid baseline be improved?
Why the pandemic’s quiet rewiring of daily life is now showing up in bodies, clinics, and aging
This piece isn’t about the pandemic itself, but about what it quietly changed in our bodies after it ended. – Dr Caplan
What You’ll Learn in This Post
❇️ How the post Covid baseline quietly altered social stamina, mood, and the cognitive cost of being around other humans.
❇️ Why weak social ties matter to human physiology and why their disappearance is a silent risk factor in aging.
❇️ How delayed care, self-triage, and long Covid now shape clinic visits more than most clinicians admit.
❇️ Where cannabis and the endocannabinoid system actually fit into the post Covid baseline rather than sitting outside of it.
❇️ Why seniors absorbed the heaviest share of these aftershocks and why Medicare cannot keep pretending otherwise.
Naming the Post Covid Baseline We’re All Living In
There was no closing ceremony. No collective decompression. No national debrief on what prolonged vigilance does to a nervous system. The country simply shifted from pandemic mode to complication mode, and the rest was left to individuals to metabolize on their own.
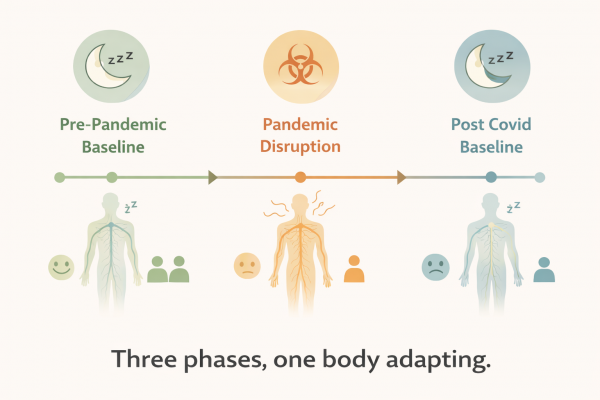
Somewhere in that transition, a new default settled in. The post Covid baseline is not a diagnosis, nor a syndrome, nor a syndrome disguised as a personality trait. It is a broad reconfiguration of how humans are now moving through the world after two years of physical isolation, digital substitution, biological threat, and a healthcare system stretched to transparency.
For many people the post Covid baseline feels like a subtle but stubborn shift in how much life can be carried without fraying. Socializing now has a price. Leaving the house requires deliberation. The body holds more tension than it can analytically justify. Rest feels thinner. Symptoms feel stickier. Optimism requires intention rather than arriving spontaneously.
On paper, most of this does not register. Tests are normal. Imaging reassures. Clinicians say things like “your labs are fine” and patients say things like “then why do I feel like this.” The chart cannot capture the nervous system’s attempt to reorganize itself after prolonged uncertainty. It can only register disease, and the post Covid baseline is not disease, it is drag.
Public Life Got Strange and No One Knows How to Name It
Of all the changes the pandemic produced, the strangest might be in how humans now relate to the public world. We had two years where being around strangers was reclassified from ordinary to suspicious, and then we were expected to reverse the classification overnight.
People did return to gatherings, restaurants, concerts, conferences, airports, and offices. But the return was tentative and often conditional. A subtle calculation sits behind many invitations: “Do I have it in me for this today.” Social stamina is now a variable rather than a constant.
There is a quiet absurdity to the new rituals of participation. Events that once required nothing more than interest now require interest plus energy plus planning plus resilience. For many, the RSVP button has become a kind of mirror.
In the pre-pandemic world, boredom was the obstacle to social life. In the post Covid baseline, the obstacle is capacity. It is not that people became antisocial, it is that public life became cognitively expensive.
Clinically this shows up as a pattern that is easy to miss. Patients describe feeling “off” or “tired” or “less motivated” or “more anxious around people,” but rarely identify it as a shift in social stamina. To them it feels personal. To clinicians it often sounds psychological. To anthropology it is neither, it is an adaptation to prolonged threat that the nervous system has not fully reversed.

Weak Ties Vanished and Health Became Harder to Detect
Before the pandemic, most people participated in a quiet lattice of relationships that sociologists call weak ties. These are not friends, they are the people who populate your surroundings and create the subtle hum of belonging. The barista who knows your face, the neighbor on the same walking schedule, the usher at church, the woman in your tai chi class. They are the background characters of a healthy social world.
The pandemic wiped them out with brutal efficiency. When it was over, strong ties mostly returned, but weak ties did not. They require proximity, repetition, and low stakes, and the post Covid baseline is poor soil for all three.
From a health perspective, weak ties serve two purposes. First, they buffer loneliness without triggering the pressures of intimacy. Second, and more importantly, they detect change. Weak ties are often the first to say things like “you look tired,” “you are limping,” “you missed last week,” or “you do not seem like yourself.” Primary care physicians often rely on families for these observations. Before the pandemic, society provided them for free.
Remove weak ties and the first line of detection disappears. Problems that would have been noticed socially are now only noticed medically, and usually later. This is particularly punishing for older adults, whose health signals are often subtle before they are urgent.
In clinics, this has produced a version of delayed discovery. By the time symptoms surface to medicine, they have already had time to entrench. The post Covid baseline did not invent frailty, depression, or cognitive decline. It simply removed the social tripwires that once caught them early.
Self-Triage Became the New Primary Care
During the pandemic, people were taught to manage symptoms at home, to avoid emergency rooms unless necessary, and to evaluate risk through apps, dashboards, and informal networks. The line between public health advice and self-management blurred.
That logic did not vanish when restrictions lifted. It simply shifted focus. In the post Covid baseline, many people run a silent calculus before seeking care. They wait. They monitor. They Google. They tighten routines. They hope it resolves. When it does not, they wait longer.
Clinicians are seeing the outcome. Problems are arriving later in their arc. There is more complexity at first presentation. There is more confusion about when symptoms began. People are less certain about what is normal for them and what is new.
Cannabis enters here as an adaptation. For some, it is for sleep. For others, anxiety. For others, pain. There is no mystery in this. Humans will medicate discomfort long before they are willing to medicalize it. Cannabis is simply a tool that is widely accessible, socially tolerable, and physiologically versatile.
In some cases, cannabis delays escalation by lowering symptom volume until patients can get care. In other cases, cannabis delays escalation by lowering symptom volume so they do not. Both patterns are rational in a world where medical access feels costly and the post Covid baseline normalizes feeling slightly unwell most of the time.

The Post Covid Baseline Lives in the Nervous System
If the pandemic rearranged anything, it was vigilance. Humans are not built for multi-year threat monitoring. The nervous system can activate quickly and deactivate slowly, but it does not deactivate gracefully when the threat is ambiguous or ongoing.
During Covid, threat was everywhere and nowhere. It was in the news, in the air, in the grocery store, in the bodies of strangers and family. You could silence the alerts on your phone. You could not silence the alerts in your limbic system.
That kind of prolonged activation has consequences. Sleep becomes lighter. Startle becomes sharper. Fatigue becomes less responsive to rest. Mood becomes less spontaneous. Symptom perception becomes louder. The post Covid baseline is not only cultural, it is neurophysiological.
The endocannabinoid system sits inside this architecture. It is the body’s internal regulator for mood, sleep, pain, appetite, and immune tone. It helps decide how loudly the nervous system broadcasts threat. During prolonged stress, it spends enormous energy dampening signals so the organism can continue functioning. It does not do so indefinitely without cost.
None of this requires exotic science to explain. When a nervous system is taught to expect uncertainty, it will continue expecting it until it has enough contradictory evidence to stand down. Most people have not had that evidence. The post Covid baseline therefore persists, not because the pandemic is ongoing, but because uncertainty is.
Long Covid: The Concentrated Version
There is a separate category of people who never returned to any baseline at all. Long Covid takes the post Covid baseline and places it into high relief. Fatigue, dysautonomia, brain fog, unrefreshing sleep, tachycardia, temperature sensitivity, exertion crashes. These are the symptoms of a nervous system and immune system struggling to coordinate under novel strain.
Long Covid reveals something the broader culture tries to ignore. When recovery is incomplete, life does not pause. People keep working, keep caregiving, keep pretending. The nervous system absorbs the slack. The bill arrives later.
In clinic, these patients tend to present with complexity that predates the appointment. By the time medicine sees them, they have already restructured their routines. They have developed coping strategies. Cannabis sometimes enters here as a tool of self-stabilization. Small doses can smooth pain, soften hyperarousal, and improve sleep onset. Higher doses can worsen cognitive fog, flatten motivation, or make pacing harder.
The tragedy of long Covid is not only biological. It is cultural. Our society is not built for illnesses that do not resolve. It is built for injuries you can point to and diseases that have protocols. Long Covid has neither. It is an edge case of the post Covid baseline where the return-to-normal story collapses and the organism is left to improvise.
Clinicians Are Living in This Baseline Too
The healthcare system did not exit the pandemic unscathed. Clinicians absorbed a level of demand and grief that the system is not designed to metabolize. Many worked through crisis conditions with no psychological decompression. The culture of medicine rewards endurance, not integration.
The result is a quiet erosion of clinical bandwidth. There is less patience for complexity. There is less time for nuance. There is more exhaustion beneath the surface. The post Covid baseline is not just for patients, it is for everyone in the exam room.
When a patient enters with tangled symptoms, a clinician with a frayed baseline may not have the capacity to deconstruct them. The clinical impulse becomes triage rather than curiosity. The system becomes transactional rather than interpretive. The organism becomes a list of problems rather than a story.
This is not a critique of clinicians. It is a critique of a system that expects them to absorb societal trauma without acknowledging it. The pandemic did not just create more patients. It created fewer clinicians with capacity for complexity. The post Covid baseline is therefore bidirectional. It shapes those who seek care and those who provide it.

Older Adults as the Cultural Canary
If there is a group that absorbed more of the post Covid baseline than anyone else, it is older adults. They lost weak ties, daily structure, embodied meaning, and social monitoring all at once. For many, routines evaporated and did not return. Choirs shrank. Card games dissolved. Senior centers reopened at half strength. Participation became conditional and then optional and then minimal.
For older adults, social life is not recreational. It is regulatory. It maintains cognitive function, mood, mobility, appetite, and orientation. When social worlds collapse, bodies follow. Decline does not scream, it accumulates.
Medicare was not built for this. It was not designed for prolonged social erosion. It was built for acute events, discrete diagnoses, episodic interventions, and reactive care. It has codes for strokes and hospitalizations and joint replacements. It has no codes for meaning, dislocation, or prolonged isolation. The post Covid baseline does not fit a billing category, so it does not exist.
Cannabis enters aging for reasons that are rarely discussed honestly. It is not only for pain or sleep or appetite. It is for easing the friction of a life that has quietly lost structure. It is for softening the dread of unstructured time. It is for making discomfort tolerable enough to function. Sometimes it works. Sometimes it merely delays reckoning. Both are adaptations to a world that has stopped scaffolding older adults.
The indictment here is not against older adults. It is against a society that expects them to build their own social infrastructure without tools, budgets, or mobility. If young adults lost events and networks during the pandemic, older adults lost the environments that made life coherent.

Where Cannabis and the ECS Fit in the Post Covid Baseline
Cannabis sits inside the post Covid baseline as both coping strategy and physiological instrument. It is neither inherently solution nor inherently distraction. It is a modulator.
For some, cannabis restores sleep that stress has fractured. For others, it reduces the bodily noise of chronic vigilance enough to re-enter social life. For others, it pulls pain back into the background where it once lived before isolation made it loud.
The endocannabinoid system explains why cannabis is so versatile here. It does not target one symptom, it tunes networks. Mood, sleep, pain, appetite, immune tone. These are the exact domains the post Covid baseline disturbs. It is not surprising that cannabis use increased during and after the pandemic. It is surprising that we pretend not to understand why.
The risk is in confusing relief with repair. Cannabis can lower the volume of symptoms long enough for people to function. It cannot rebuild weak ties, redesign Medicare, or reverse long Covid. It is a tool, not a world.
The opportunity is in using cannabis deliberately inside a broader architecture of recovery rather than as a solitary intervention. That requires clinicians who can ask the right questions and patients who can answer them without fear of judgment. It also requires acknowledging that the post Covid baseline is not an individual failure, but a societal one.
What to Do with a Baseline You Did Not Choose
The hardest part of the post Covid baseline is that it arrived without consent. People did not choose to become less social, less rested, less flexible, less optimistic, or more symptomatic. The baseline shifted and the organism adapted.
The good news is that baselines are not destiny. They are just defaults. They can be examined, questioned, modified, and rebuilt. The first step is to stop treating them as personality traits. When someone says “I am just this way now,” they are often naming resignation, not identity.
Clinically, there are leverage points. Small social re-entry, not for entertainment but for regulation. Sleep routines that respect nervous system timing rather than caffeine and despair. Cannabis used with intention rather than autopilot. Care sought before crisis rather than after it. Conversations with clinicians that include stories, not just symptoms.
None of this returns us to a pre-pandemic world. There is no return. There is only forward movement with better tools. The post Covid baseline is not the end of the story. It is the setting. What people do with it depends on whether they recognize it as malleable.
The organism is built to adapt. Society is slower. Medicare is even slower. Cannabis is just one instrument among many. But the body listens to all instruments at once. The question for the coming decade is whether the systems that surround the body will learn to listen too.
FAQS about the new Post-COVID Baseline
1. What is the post Covid baseline?
The post Covid baseline refers to the new default state many people settled into after prolonged pandemic stress, disruption, and uncertainty. It is not a disease, but a shift in nervous system regulation, social stamina, and symptom tolerance. People often notice more fatigue, lighter sleep, and less capacity for social engagement. Because it developed gradually, many mistake it for aging or personality change. Naming it helps clinicians and patients respond more intelligently.
2. How does the post Covid baseline affect mental health?
The post Covid baseline often amplifies anxiety, low mood, irritability, and cognitive fatigue. Prolonged vigilance trains the nervous system to stay partially activated, even when danger has passed. This makes rest less restorative and stress more persistent. Many people feel emotionally “flat” rather than acutely distressed. That subtlety is why it often goes unaddressed.
Social life became cognitively expensive during the pandemic, and that cost did not fully reset. Reduced practice, ongoing uncertainty, and diminished weak ties all contribute. In the post Covid baseline, people tire faster in public settings and require more recovery afterward. This is not antisocial behavior, it is a nervous system adaptation. With gradual reentry, capacity can often be rebuilt.
4. What are weak ties and why do they matter for health?
Weak ties are casual social connections like neighbors, classmates, or familiar staff at local places. They provide social buffering and early detection of change. When weak ties disappeared during the pandemic, subtle health declines went unnoticed longer. This delayed recognition affects both mental and physical health. Older adults are particularly vulnerable to this loss.
5. How did Covid change healthcare-seeking behavior?
The pandemic normalized self-triage, home monitoring, and delayed care. In the post Covid baseline, many people wait longer before seeing clinicians. This results in later-stage presentations and more complex symptom patterns. While understandable, this delay can increase health risks. Early conversations often lead to simpler interventions.
6. What is the relationship between long Covid and the post Covid baseline?
Long Covid is a more concentrated version of baseline disruption. It features persistent symptoms that do not fully resolve after infection. The post Covid baseline applies more broadly, including people without clear long Covid diagnoses. Both involve nervous system dysregulation and prolonged adaptation. Care requires patience, nuance, and flexibility.
7. How does the nervous system play a role in post Covid symptoms?
The nervous system governs threat detection, rest, sleep, and symptom perception. During prolonged uncertainty, it remains partially activated. This leads to fatigue, sleep disruption, and heightened symptom awareness. The post Covid baseline reflects this ongoing activation. Calming the nervous system is often central to recovery.
8. Where does cannabis fit into the post Covid baseline?
Cannabis interacts with the endocannabinoid system, which regulates mood, sleep, pain, and immune tone. In the post Covid baseline, cannabis may reduce symptom intensity and support function. Used thoughtfully, it can be helpful. Used indiscriminately, it may mask deeper issues. Clinical guidance improves outcomes.
9. Why were seniors affected more by post Covid changes?
Older adults lost routine, social monitoring, and embodied meaning during the pandemic. Many of those supports never fully returned. Because social life regulates cognition and mobility in aging, decline accelerated quietly. Medicare is poorly designed to address this kind of erosion. Seniors became the earliest signal of systemic strain.
10. Can the post Covid baseline be improved?
Yes, baselines are defaults, not destinies. With intentional social reentry, nervous system support, sleep optimization, and thoughtful care, many people improve. Cannabis may play a role when used deliberately. The key is recognizing the baseline shift rather than resigning to it. Awareness creates agency.
