Table of Contents
- Medical Cannabis Crossroads: 5 Alarming Shifts in Care
- What You’ll Learn in This Post
- Evidence in this blog is grounded in
- From fringe to front door: how we arrived at the medical cannabis crossroads
- When medical cannabis behaved like actual medicine
- Medical cannabis crossroads: when adult-use opened the side door
- From stewards to card mills: when “medical” becomes a membership
- What disappears when the follow-up visit vanishes
- The hemp bridge and the federal storm heading for it
- What is really at stake at the medical cannabis crossroads
- Choosing the road that keeps medicine human
- References and Evidence Base
- Medical Cannabis Crossroads FAQ
- What is the “medical cannabis crossroads” everyone is talking about?
- Why are medical cannabis registries shrinking in adult-use states?
- If adult-use cannabis is legal, what unique value does medical cannabis provide?
- Are “card mill” clinics really that big of a problem?
- What does the evidence actually say about cannabis and opioid reduction?
- How will the new federal hemp THC limit affect people who use hemp products for sleep or anxiety?
- What can patients do to protect themselves at the medical cannabis crossroads?
- How should clinicians respond if they feel unprepared to talk about cannabis?
- Is medical cannabis still an attractive area for long term investment?
- What would a healthy future beyond the medical cannabis crossroads actually look like?
Medical Cannabis Crossroads: 5 Alarming Shifts in Care
Medical cannabis is standing at a crossroads. On one side is fast, frictionless access that treats the plant like a coupon. On the other is slower, more deliberate care that treats it like medicine. Which road we choose will quietly shape how much suffering we accept as inevitable in the years ahead.
What You’ll Learn in This Post
❇️ How the medical cannabis crossroads emerged from twenty years of rapid growth, policy shifts, and quiet exits from care
❇️ Why medical cannabis enrollment is shrinking in many adult-use states even while cannabis sales soar
❇️ How “card mills” and coupon culture hollow out the deeper medical value of cannabis
❇️ How the new federal hemp crackdown collides with a medical system that is already thinning out
❇️ What patients, clinicians, and investors can still choose if they care about real healing, not just transactions
Evidence in this blog is grounded in
• A national observational study in Annals of Internal Medicine showing that U.S. medical cannabis enrollment increased about 4.5-fold from 2016 to 2020, with enrollment declining in states that adopted adult-use laws
(Boehnke et al., 2022).
• A follow-up analysis covering 2020 to 2022 showing that medical cannabis registrations continued to grow overall but generally decreased in jurisdictions with adult-use markets, while chronic pain, anxiety, and PTSD remained the leading qualifying conditions
(Boehnke et al., 2024).
• Clinical survey data in chronic pain populations linking medical cannabis use with meaningful reductions in opioid use, fewer medication side effects, and improved quality of life, including an average 64 percent reduction in opioid doses in one cohort
(Boehnke, Litinas, Clauw, Journal of Pain, 2016).
• Massachusetts Cannabis Control Commission open data and press releases documenting more than 8 billion dollars in cumulative adult-use cannabis sales through mid 2025, alongside a roughly 40 percent decline in annual medical sales since a 2021 peak and ongoing closures or sales of medical dispensaries
(Massachusetts Cannabis Control Commission, 2025,
Cannabis Business Times, 2025,
Axios Boston, 2025).
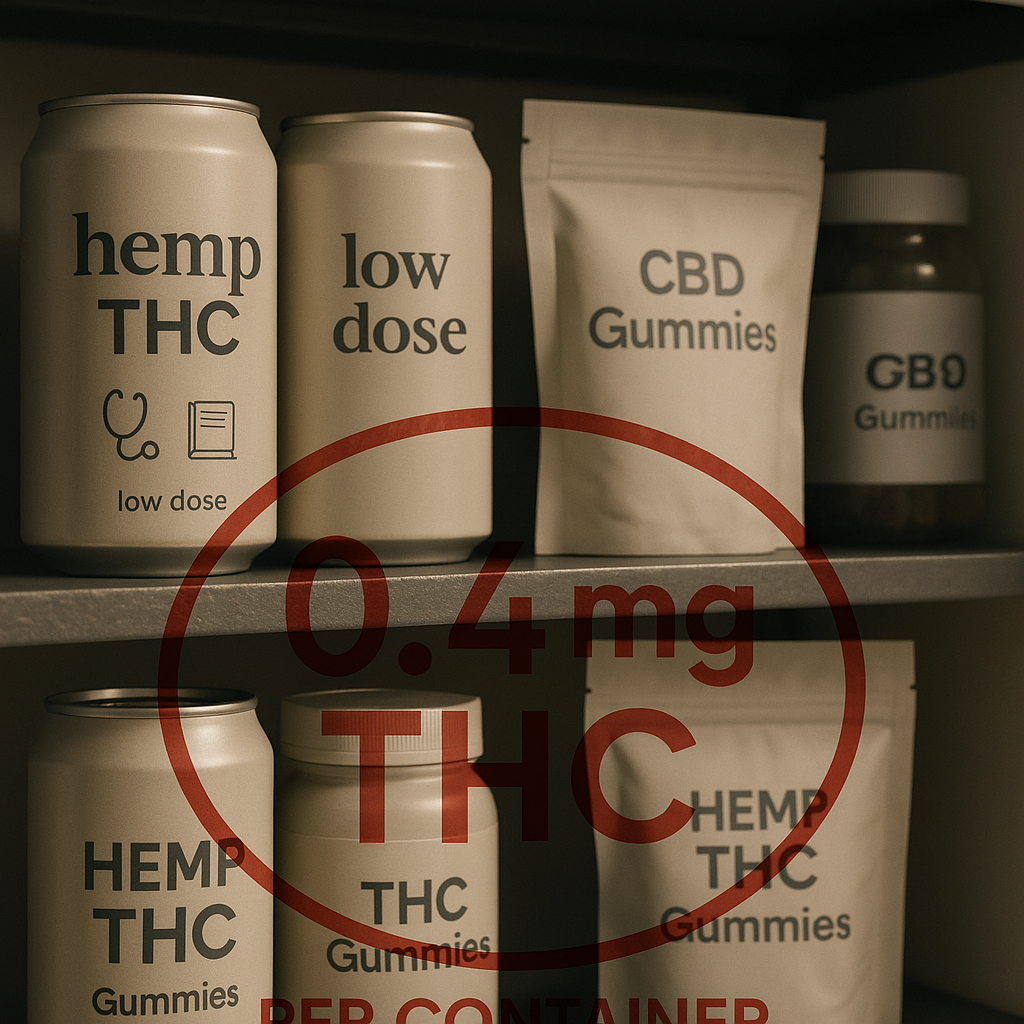
• Congressional and legal analyses of new federal legislation redefining hemp and capping total THC at 0.4 milligrams per container in finished products, together with national reporting on how the ban will remove most intoxicating hemp edibles and beverages from interstate commerce by 2026
(Congressional Research Service, 2025,
DLA Piper, 2025,
The Guardian, 2025).
From fringe to front door: how we arrived at the medical cannabis crossroads
Twenty years ago, the idea of a dedicated medical cannabis clinic felt like something from a parallel universe. Most of the people who talked about cannabis used whispered slang and jokes, not medication lists and symptom diaries. Then, almost overnight and very slowly all at once, the landscape changed.
By 2016, state registries were tracking hundreds of thousands of people who had taken the risk of saying, out loud, that cannabis helped them function. By 2020, enrollment in medical cannabis programs had increased more than fourfold compared to 2016, as patients and clinicians gradually discovered that the endocannabinoid system was not a trivial side character but a storm-balancing network threaded through pain, mood, sleep, immunity, appetite, and memory. (Years later, registry analyses in Annals of Internal Medicine would quantify that same surge, confirming what many clinics were seeing in daily practice.)
Much of that growth was driven by chronic pain, anxiety, and trauma. The official numbers tell that story in a dry way. In 2020, chronic pain was the dominant qualifying condition across the United States, and by 2022 it remained the single most common reason people entered medical cannabis programs, with anxiety and post-traumatic stress not far behind. (Those patterns map almost perfectly onto the registry data, where chronic pain sits at the top of the list and anxiety and PTSD cluster closely behind.) Behind those labels were people who could no longer sleep through the night, parents who could not stay in the room with their children’s chaos without snapping, and patients who had run out of medications that helped more than they harmed.
Enrollment in medical cannabis programs increased about 4.5-fold from 2016 to 2020 across the United States, with chronic pain, anxiety, and PTSD leading the list of indications in national registry reports.
In exam rooms, the change was even more obvious. People walked in carrying pill bottles and weariness. Many had already tried physical therapy, injections, surgeries, or sleep medications that left them foggy and flat. They asked some version of the same question: “I am not sure who I am underneath all of this. Could cannabis help me find my way back to myself?”
At that point, medical cannabis still felt like medicine. Not perfect, not magic, but recognizably clinical. Visits were long, sometimes messy. We talked about THC and CBD as tools instead of trophies, microdoses instead of moon shots, and the peculiar way the medical cannabis crossroads was beginning to form even before we had a name for it.

When medical cannabis behaved like actual medicine
In those early years, the medical cannabis crossroads was still far off in the distance. The work felt new and slightly improvised, but grounded in a simple idea: if we understood the endocannabinoid system and respected the rest of the body, we might help people suffer less without numbing them into strangers.
A woman with migraines that taught her children to whisper came in carrying a plastic bag of failed prescriptions. A veteran whose nervous system flinched at every loud sound wanted to know whether there was a way to feel steady without feeling sedated. A man who had finally quit alcohol asked, very quietly, whether there was another way to calm his evenings that did not involve slipping back toward the bottle.
We started low, with doses that felt almost offensively small. One or two milligrams of THC at night. A steady background of CBD. Careful changes in timing. We talked about intention, about noticing what pain felt like when it was turned down just enough that you could move toward it instead of away, and about the difference between escaping your life and re-entering it.
Later, when I finally checked the numbers in the journals, the trend was unmistakable, and eerily similar to what my waiting room already knew. In a survey of chronic pain patients in Michigan, medical cannabis use was associated with an average 64 percent reduction in opioid use, fewer medication side effects, and improved quality of life. In another analysis, more than one third of medical cannabis patients who used opioids achieved at least a 30 percent reduction in their daily opioid dose. (These findings, published in The Journal of Pain, gave a peer reviewed backbone to the quiet shifts many patients were already describing in their own kitchens and bedrooms.)
Across several chronic pain cohorts, medical cannabis use has been linked to substantial reductions in opioid dose, with many patients reporting better pain control and fewer side effects when cannabis is used thoughtfully alongside or instead of opioids.
I did not need those statistics to recognize a different kind of relief in front of me. People cried less, laughed more, slept longer, and reported fewer evenings they wanted to drink themselves numb. They did not become new people. They became slightly more themselves.
That is what real medicine often does. It does not turn life into a postcard. It restores enough balance that you can stand inside your own story without feeling like you have to bolt. For a while, medical cannabis fit that description. The medical cannabis crossroads was visible only as a faint line on a distant horizon.

Medical cannabis crossroads: when adult-use opened the side door
Then adult-use legalization arrived, not as a single event but as a series of votes and ribbon cuttings. At first, it felt like a simple victory. Fewer arrests. Less stigma. More honesty about a plant that had been hiding in everyone’s blind spot for decades.
Patients celebrated. Many clinicians did too. You no longer had to carry the awkward weight of being “the cannabis patient” just to buy something that helped you sleep. You could walk into a store with the anonymity of any other consumer. No exam room. No forms. No waiting for a physician who might or might not understand what you were trying to do.
What my waiting room sensed long before I had words for it was eventually confirmed by multi-state registry analyses and industry data. When adult-use sales begin, medical cannabis enrollment reliably falls. On average, states see medical registries shrink by about one third after recreational markets open, with some jurisdictions losing more than half their registered patients within a few years. (Those declines show up clearly in the registry trend lines published in Annals of Internal Medicine when adult-use laws take effect.)
Analyses of medical cannabis registries show that once adult-use markets launch, medical enrollment declines by roughly one third on average, with some states losing more than half of their registered patients within a few years.
In Massachusetts, adult-use sales crossed the 8 billion dollar mark by mid 2025. At the same time, annual medical sales fell about 40 percent from a 2021 peak. The plant was not disappearing. The structure of care around it was. (State open data and trade coverage from the Cannabis Control Commission, Axios, and Cannabis Business Times all tell the same story of booming adult-use revenue alongside a shrinking, consolidating medical market.)
In Massachusetts, adult-use cannabis sales have exceeded 8 billion dollars since 2018, while annual medical sales have dropped from roughly 270 million dollars in 2021 to about 160 million in 2024.
Stand in a busy adult-use dispensary, and the medical cannabis crossroads looks like progress. The store is full of customers, the tax revenue is impressive, and the stigma is lower than it has been in decades. Stand in a clinic that used to see patients back for careful second and third visits, and it looks like something else entirely.
Fewer follow-ups. More one-time visits. More patients who come once to talk about replacing sleeping pills or alcohol, then quietly vanish into the adult-use marketplace to experiment alone. The shift was not anecdotal. It was measurable, persistent, and seen everywhere adult-use took root.
From stewards to card mills: when “medical” becomes a membership
Economics has a way of bending the spine of any system, especially one that sits at the crowded intersection of medicine, stigma, politics, and profit. The medical cannabis crossroads is no exception.
Thoughtful medical care takes time. A 45-minute visit that includes a full medication review, a trauma history, a sleep map, and a realistic discussion of goals is hard to sustain when insurance rarely pays for it and when patients can bypass the process by walking into an adult-use shop.
So some medical cannabis practices adapted. They shrunk the time, simplified the questions, and optimized the workflow around one primary task: generating or renewing cards. Marketing followed. “Same-day approvals.” “No records needed.” “Fastest renewal in the state.” The medical card quietly shifted from the symbol of an ongoing clinical relationship into something closer to a membership card at a warehouse club.
Many patients now talk about their medical card in exactly those terms. You pay a fee, often a few hundred dollars a year between state and clinician costs, and the primary benefits are lower taxes, bigger purchase limits, and access to certain products on the medical side of a hybrid store. The substance of the visit starts to feel secondary. (In patient surveys, people who abandon medical programs frequently cite cost and bureaucratic hassle rather than disappointment with cannabis itself or lack of benefit.)
Clinics that resist this drift still exist. At places like CED Clinic, for example, visits are structured around education and follow-up, not only signatures. Patients come not just for a card, but for help choosing between dosing strategies, delivery methods, and long-term plans. That approach is visible in educational pieces like cannabis for anxiety, cannabis for sleep, and the clinical overview of the expanded endocannabinoid system, which treat cannabis as a tool to be understood, not a commodity to be grabbed.
But the larger trend is hard to ignore. As more “card mills” appear and more patients see their medical card primarily as a discount coupon, the physician’s role as steward begins to evaporate. At the medical cannabis crossroads, the white coat stays on, but the soul of the work starts to drain away.
Surveys of patients leaving medical programs often cite cost, bureaucracy, and lack of perceived extra value compared with adult-use access, rather than dissatisfaction with cannabis itself.
You cannot be both a coupon and a compass for very long. Eventually, one of those roles wins.
What disappears when the follow-up visit vanishes
The most important work in medical cannabis rarely happens at the first visit. The first visit is the part where everyone is polite and slightly guarded. Patients show you their diagnosis problem list, their medication list, and the story they have learned to compress into ten minutes for insurance-driven medicine.
The second or third visit is different. That is where the medical cannabis crossroads becomes visible at human scale.
By then, the dosing plan has lived in the real world for a few weeks. Sleep has either deepened or not. Pain has either shifted or stubbornly clung to the same corner of the body. Alcohol and sedative use may have shrunk, stayed the same, or quietly crept up again. Patients arrive with more honesty and more curiosity, because they have seen enough change to know that their own behavior matters.
“This is going to sound strange,” one patient told me eight weeks into a carefully planned trial of low-dose THC and CBD at night, “but I feel like I am starting to meet my life again. Same job, same kids, same stress. Just less dog-face, frog-face, bog-face in my head about every little thing.”
Another, a man with years of back pain and a long opioid history, said, “We cut my dose in half and I did not fall apart. I still hurt, but I am less afraid of the pain. My wife says I actually listen at dinner.” (These are exactly the kinds of stories that sit underneath the percentage drops in opioid use and quality of life scores in the chronic pain surveys.)
These sentences do not appear in registry reports. They do not show up in quarterly revenue statements. But they are exactly the kind of outcome that clinical studies hint at when they show reductions in opioid use and improvements in quality of life among medical cannabis patients who receive structured guidance.
When patients leave medical programs and rely only on adult-use or informal markets, they rarely receive any ongoing support around dose, timing, interactions, or goals, even though these elements strongly influence outcomes.
When the follow-up visits vanish, several things disappear at once. The chance to correct a dose that is too high, too frequent, or poorly timed. The opportunity to notice that someone’s alcohol intake is creeping upward again as they rely on cannabis less skillfully. The moment when a patient realizes that what they want is not endless escape, but the ability to stay present for the life they already have.
Without that space, cannabis slides from “medicine that helps me change” into “product that helps me cope.” That shift is subtle on paper, but enormous in a kitchen at midnight when someone is deciding whether to reach for a gummy, a drink, a pill, or a screen.
The hemp bridge and the federal storm heading for it
While state medical and adult-use systems have been evolving, a third quiet channel has been carrying millions of people across their own private medical cannabis crossroads: hemp-derived products.
Since the 2018 Farm Bill, CBD oils, softgels, creams, and an expanding universe of hemp-derived THC beverages and edibles have seeped into supermarkets, online storefronts, and neighborhood shops. For people in prohibition states or in regions far from dispensaries, these products have functioned as a kind of gray-market medical system. Not perfect, not consistently labeled, but present.
Many patients who never enrolled in a state program found their way to sleep with a 2 milligram hemp “nightcap” drink or a low-dose gummy. Others used CBD for arthritis or anxiety while waiting for their state to modernize its laws. In that sense, hemp created an improvised, consumer-driven version of the medical cannabis crossroads.
That bridge is now under heavy construction. Recent federal legislation has narrowed the definition of legal hemp and set an upper limit of 0.4 milligrams of total THC per finished product container. Most intoxicating hemp-based gummies, chocolates, and beverages on the market today contain far more than that, which means they will effectively vanish or be reformulated into something unrecognizable by the time the law is fully in force. (Policy analysts at the Congressional Research Service and legal commentators at firms like DLA Piper highlight this 0.4 milligram cap as the central change that will sweep most current hemp THC products off mainstream shelves.)
A national hemp market worth tens of billions of dollars, including many low-dose THC drinks and edibles, now faces strict caps of 0.4 milligrams of THC per container, which will effectively remove most intoxicating hemp products from interstate commerce.
At the same time, federal rules are tightening around synthetic or chemically converted cannabinoids like delta 8 and delta 10, closing the farm bill loophole that allowed them to flourish. For many in the regulated cannabis industry, this feels like overdue clarity. For patients in states without strong medical cannabis infrastructure, it feels like a trap door opening under their feet. (National coverage in outlets such as The Guardian has already begun describing this as a coming “hemp ban” for everyday consumers.)
The timing matters. The hemp crackdown is arriving just as medical cannabis programs in many adult-use states are thinning and shifting toward card mills, not comprehensive care. That means millions of people could lose access to hemp-derived products and still have no realistic way to obtain guided medical cannabis. The medical cannabis crossroads is not just about one system. It is about three partially overlapping systems drifting in dangerous directions at the same time.
Without strong medical cannabis programs, the combination of a hemp crackdown and adult-use convenience may leave many patients with legal products but no meaningful clinical support, or with restricted products and a return to older, more harmful coping strategies.
What is really at stake at the medical cannabis crossroads
When people talk about the decline of medical cannabis, they often focus on the visible parts. Fewer cards issued. Lower registry counts. Consolidation of clinics. Shrinking margins. If you stand at the medical cannabis crossroads from a distance, it looks like the end of a business model.
Up close, it is something else. It is a slow reduction in the number of places where you can talk about cannabis and suffering in the same breath without embarrassment. It is fewer rooms where someone will ask you why you reach for wine, or how many medications you actually want to take if other strategies exist. It is fewer opportunities to suggest that maybe, just maybe, the goal is not to eliminate every unpleasant sensation, but to change your relationship with them.
Medical cannabis at its best is not a replacement for every pill. It is a wedge in the door of a very rigid medical model, a reminder that the body has more than serotonin and opioid receptors, and that people have more than two options: “take this and ignore your feelings” or “tough it out and try to be grateful.” It invites questions like: Do I still need this benzodiazepine if I am sleeping again? What happens to my drinking when I am less anxious in my own skin? What if healing is not just about symptom scores, but about returning to the version of myself I want to live with?
If the field at the medical cannabis crossroads continues to drift toward coupons and card mills, we lose both short-term and long-term value. Short term, we lose education and stewardship. Long term, we lose one of the few mainstream tools that can challenge our dependence on polypharmacy, alcohol, and numbing as the default responses to an overwhelming world.
That loss will not show up all at once. It will look like slightly more insomnia, slightly more anxious evenings, slightly more people who feel trapped between suffering and sedation. It will look like patients deciding that “nothing works” when what they really lost was the guidance that helped them use existing tools well.
Choosing the road that keeps medicine human
The hopeful part of the medical cannabis crossroads is that it is still a crossroads. None of this is fully baked into the future. Patients, clinicians, and investors have more influence than they might think.
Patients can treat cannabis as medicine even when they buy it in adult-use settings. They can keep simple logs of dose, timing, and effect. They can track how sleep, pain, mood, and alcohol or medication use shift over weeks, not just hours. They can seek out clinicians and resources that take the endocannabinoid system seriously, such as the educational materials at CED Clinic or accessible frameworks like The Doctor-Approved Cannabis Handbook.
Clinicians can decide that learning this physiology is part of modern medicine, not a fringe hobby. They can read the same registry analyses and pain studies that patients quote in waiting rooms. They can ask about cannabis the way they ask about alcohol and tobacco, not to punish, but to understand. They can say, very simply, “If you are going to do this, I would rather help you do it safely.”
Investors and industry leaders can choose to build businesses that reward outcomes and education, not only velocity. That means supporting clinics that integrate telehealth with dispensary visits, funding outcome tracking that does more than count units sold, and building systems that make follow-up straightforward rather than an afterthought.
None of that will be as instantly profitable as minting new discount cards. It will, however, be more durable and more defensible. The companies and clinics that survive the next decade at the medical cannabis crossroads are likely to be the ones that can look regulators, patients, and clinicians in the eye and say, “We did not just move product. We helped people change.”
I do not believe medical cannabis is dying. I believe it is being asked a hard question. Are you content to be a coupon, or do you want to be a craft. The registry graphs and sales data can tell us which way the money is flowing. The exam rooms and kitchen tables will tell us which way the meaning is flowing.
If we are careful, we can still choose the road where cannabis remains a well-studied, well-guided tool in the larger work of healing. Where data and stories keep each other honest. Where medicine is not just about reducing numbers on a chart, but about helping people feel like they belong in their own lives again.
References and Evidence Base
-
Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL.
US Trends in Registration for Medical Cannabis and Reasons for Use From 2016 to 2020.
Annals of Internal Medicine.
2022;175(9):1280-1288. doi:10.7326/M22-0217. -
Boehnke KF, Sinclair R, Gordon F, et al.
Trends in U.S. Medical Cannabis Registrations, Authorizing Clinicians, and Reasons for Use From 2020 to 2022.
Annals of Internal Medicine.
2024;177(4):458-466. doi:10.7326/M23-2811. -
Boehnke KF, Litinas E, Clauw DJ.
Medical Cannabis Use Is Associated With Decreased Opiate Medication Use in a Retrospective Cross-Sectional Survey of Patients With Chronic Pain.
The Journal of Pain.
2016;17(6):739-744. -
Massachusetts Cannabis Control Commission.
Massachusetts Marijuana Establishments Pass $8 Billion in Gross Adult-use Sales.
Press release and open data portal.
July 22, 2025.
Available at:
Massachusetts Cannabis Control Commission press release on $8B adult-use sales
. -
Solis S.
Massachusetts’ medical cannabis market shrinks as patients call for reforms.
Axios Boston.
May 8, 2025.
Available at:
https://www.axios.com/local/boston/2025/05/08/massachusetts-medical-cannabis-market-shrinks
. -
Lange T.
Massachusetts Medical Cannabis Sales Drop 40% Since 2021 Peak.
Cannabis Business Times.
September 8, 2025.
Available at:
https://www.cannabisbusinesstimes.com/us-states/massachusetts/news/15754827/massachusetts-medical-cannabis-sales-drop-40-since-2021-peak
. -
Congressional Research Service.
Change to Federal Definition of Hemp and Implications for Hemp-Derived Cannabinoid Products.
In Focus IN12620.
November 2025.
Available at:
https://crsreports.congress.gov/product/pdf/IN/IN12620
. -
Gardner J, Mayl SL.
New federal restrictions on hemp and hemp-derived products: Top points.
DLA Piper client alert.
November 18, 2025.
Available at:
https://www.dlapiper.com/en-us/insights/publications/2025/11/new-federal-restrictions-on-hemp-and-hemp-derived-products
. -
Green HH.
What to know when the ban on most US hemp products goes into effect.
The Guardian.
December 3, 2025.
Available at:
https://www.theguardian.com/society/2025/dec/03/us-ban-hemp-products
.
🗣️ Know someone overwhelmed by caregiving for an elderly parent or friend? Dr Caplan is on a mission to step in and support this often neglected group. You can learn more here:
Caregiver Support for Seniors.
🗣️ Pediatric caregiving is a different sort of heavy. Many families caring for children with sleep, behavior, or neurologic challenges feel unseen. If you know someone who might benefit, please feel free to share our
Pediatric Care Program.
Do you know one person we could help? A quiet share can change the trajectory of a whole household.