Pregnancy pain relief, family genetics, and a controversial debate collide in modern medicine
Table of Contents
- What You’ll Learn in This Post
- Tylenol and Autism: A Debate as Tangled as Parenthood Itself
- The 2025 Super-Study That Shook the Conversation
- When Fever, Genes, and Families Muddy the Waters
- The Sibling-Control Study That Flipped the Script
- Biomarkers and Blood Clues: A Twist in the Tale
- Guidelines Haven’t Changed, and Here’s Why
- The View From My Clinic: Hundreds of Families, Endless Questions
- Public Panic vs Public Understanding
- My Take: Complexity Over Certainty
- How CED Clinic Supports Families Living With Autism
- 10 FAQ Q&A about Tylenol and Autism
- 1. Does Tylenol use during pregnancy cause autism?
- 2. What is confounding by indication, and why does it matter?
- 3. Are sibling studies more reliable than other research designs?
- 4. Why haven’t guidelines changed if there’s a possible link?
- 5. How can parents safely use Tylenol during pregnancy?
- 6. What do biomarker studies reveal about Tylenol and autism?
- 7. Are there alternatives to Tylenol for pregnancy pain?
- 8. How do media headlines distort the science?
- 9. Should pregnant people completely avoid Tylenol?
- 10. What is the future of research on Tylenol and autism?
What You’ll Learn in This Post
❇️ How acetaminophen (Tylenol) use in pregnancy became a global health debate
❇️ What the latest 2025 systematic review really found about Tylenol and autism
❇️ The hidden role of genetics, fever, and family factors in research results
❇️ Why guidelines still recommend Tylenol as the first-line pregnancy medication
❇️ Where emerging therapies, including cannabis, might play a future role in care
Tylenol and Autism: A Debate as Tangled as Parenthood Itself
Picture this: a pregnant woman sits on the edge of their bed, cradling a pounding head, a thermometer flashing a fever, a baby kicking inside. On the nightstand sits a small, familiar bottle: Tylenol.
For decades, acetaminophen has been the safe choice for pregnancy pain relief. But recent research has cracked open a question that strikes at the heart of modern parenting: Could that same pill be linked to autism or ADHD in children?
The stakes are monumental. Over half of pregnant individuals worldwide use Tylenol. Even the faintest whiff of risk sends shockwaves through families, public health agencies, and the scientific community alike. And like every modern health debate, the conversation quickly spirals from cautious curiosity into cultural chaos.
The 2025 Super-Study That Shook the Conversation
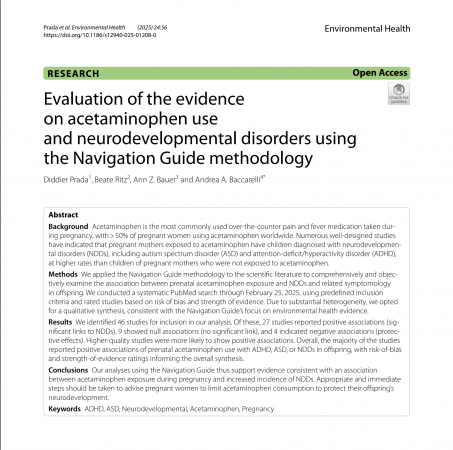
This year, Prada, Ritz, Bauer, and Baccarelli published a comprehensive systematic review in Environmental Health. Their analysis sifted through 46 human studies spanning millions of pregnancies, examining the potential connection between Tylenol and autism. The results? A scientific Rorschach test, with patterns open to interpretation rather than clear, causal answers.
27 studies reported a positive link between prenatal Tylenol use and later ADHD or autism in children. 9 studies found no connection at all. And in a surprising twist, 4 studies even hinted at a protective effect.
Faced with this messy mosaic, the authors took a bold stance: no meta-analysis.
Why? Because combining wildly different studies into one pooled number would risk false precision—like trying to average a symphony with a rock concert and calling it music. Instead, they offered a qualitative synthesis, weighing each study’s context, strengths, and flaws.
Their conclusion was carefully worded: “The evidence is consistent with an association.”
Not proof. Not panic. Just a signal worth paying attention to.
When Fever, Genes, and Families Muddy the Waters
It’s tempting to leap from “association” to “causation,” but observational research is notoriously tricky. Enter one of science’s slipperiest villains: confounding by indication.
Imagine two pregnant people:
One takes Tylenol for a mild headache.
The other takes it to lower a dangerous fever caused by an infection.
If their children later develop ADHD or autism, is the culprit the Tylenol… or the fever… or the infection itself? Or perhaps something invisible, like shared genetics? Untangling these threads is like playing a game of “dog-face, frog-face, bog-face”—silly words, serious stakes, each possibility morphing into the next before your eyes.

The Sibling-Control Study That Flipped the Script
To fight back against confounding, researchers use sibling-comparison studies, a clever design that compares siblings born to the same mother. This automatically controls for many shared genetic and environmental factors.
A 2024 JAMA study applied this approach to an astonishing 2.5 million Swedish children. When siblings were compared, the apparent link between Tylenol and autism or ADHD vanished.
No increased risk. No dramatic headlines. Just the quiet suggestion that earlier studies might have been tracing the outlines of family genetics and household environments, not a direct drug effect.
This doesn’t close the case. It cracks it wide open. It says, “Slow down. Look again.”

Biomarkers and Blood Clues: A Twist in the Tale
While most studies rely on self-reported Tylenol use (“Did you take any during pregnancy?”), a few cutting-edge investigations went deeper. They measured acetaminophen metabolites in umbilical cord blood.
These biomarker studies found something provocative: dose-response relationships. The higher the Tylenol levels in the blood, the higher the observed risk of ADHD and autism diagnoses later in childhood.
It’s like finding footprints at a crime scene. But even then, we don’t know who—or what—left them. Were those footprints evidence of Tylenol’s direct effects, or simply a marker of severe illness and fever requiring higher doses?
Guidelines Haven’t Changed, and Here’s Why
Despite this growing swirl of research, ACOG and other leading medical organizations continue to recommend acetaminophen as the first-line treatment for pain and fever during pregnancy.
The guidance is straightforward:
-
Use Tylenol only when medically necessary
-
Keep the dose low
-
Keep the duration short
-
Talk to your doctor before prolonged or frequent use
Why the continued support? Because untreated fever and severe pain also carry significant risks for mother and baby. Avoiding Tylenol entirely could do more harm than good.

The View From My Clinic: Hundreds of Families, Endless Questions
In my practice, I care for hundreds of families raising children on the autism spectrum. If there’s one truth I carry with me, it’s this: there is deep, often invisible suffering in these households.
Autism touches everything—school mornings, mealtimes, sleep, sibling relationships. Parents fight exhausting battles for services and understanding, often in silence. The science may be tangled, but the pain is plain.
Some families find relief in unexpected places, including carefully guided cannabis treatments for symptoms like anxiety, sleep disturbances, and severe behavioral outbursts. But cannabis is not a cure, and like Tylenol, it demands respect and precision.
The real work ahead isn’t to vilify one drug or glorify another—it’s to listen, to research better, and to build systems that support families no matter where the science currently stands.
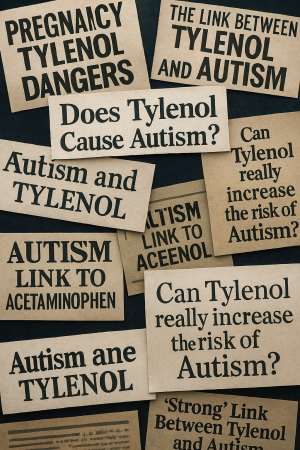
Public Panic vs Public Understanding
Here’s the problem: nuanced scientific statements don’t go viral. Headlines do.
“The evidence is consistent with an association” becomes “Tylenol causes autism!” by the time it hits social media.
This misunderstanding can lead to dangerous outcomes. Pregnant people might avoid treating high fevers, risking miscarriage or serious complications. Others might spiral into guilt years later, wondering if their choice of pain reliever shaped their child’s future.
We need a new cultural approach: one that values caution without fearmongering, and transparency without blame.
My Take: Complexity Over Certainty
Tylenol and autism. Fever and genetics. Association and causation.
This isn’t just a scientific puzzle—it’s a reflection of how messy real life is.
The story isn’t over. It may never have a tidy ending. But by embracing complexity, we move closer to truth. And by caring for families with compassion—whether through traditional medicine, cannabis-based therapies, or simply listening—we honor the lives behind the data.
More of my writing on this topic
Expecting and Experimenting (Cannabis and Pregnancy)
Pregnant & Curious: Unpacking Cannabis Myths, Risks & Research
Hyperemesis, Cannabis, and a Mother’s Courage: Ray’s Story of Survival and Advocacy
Cannabis as a Potential Solution for Metabolic Syndrome
News reports on this topic
How CED Clinic Supports Families Living With Autism
For families living with autism, there is often a deep longing for options that bring more peace and stability to daily life. At CED Clinic, we’ve had the privilege of supporting hundreds of families—from young children to adults on the autism spectrum—through guided cannabinoid therapies.
Medical cannabis isn’t a one-size-fits-all solution, and it may not be right for every family, but for many, it has opened doors to calmer nights, better communication, and a sense of hope. If you’re curious or simply exploring what’s possible, we’re here to listen, answer questions, and help you consider whether this approach might be a fit for your loved one. Sometimes, just starting the conversation can be the most important first step.
To learn more, email Jack
10 FAQ Q&A about Tylenol and Autism
1. Does Tylenol use during pregnancy cause autism?
Current evidence shows associations but not proof of causation. A 2025 systematic review found many positive links, but a massive sibling study suggests family genetics and environment may explain the connection. This means Tylenol may not be directly responsible. It’s a question still under study.
2. What is confounding by indication, and why does it matter?
Confounding by indication occurs when the reason for taking a drug—like fever or infection—affects outcomes. For Tylenol, this means it’s hard to separate the effect of the drug from the effect of the fever itself. This is a major challenge in pregnancy research. It’s like mixing up footprints at a crime scene.
3. Are sibling studies more reliable than other research designs?
Sibling studies compare children born to the same mother, controlling for shared genetics and environment. The 2024 Swedish study using this method found no link between Tylenol and autism or ADHD. While powerful, sibling studies have their own limitations. Still, they provide valuable context for interpreting associations.
4. Why haven’t guidelines changed if there’s a possible link?
Guidelines like ACOG’s continue to support Tylenol use because untreated fever and severe pain also carry risks. The evidence for harm is observational and conflicting. Until causation is proven, the balance of risks favors careful, minimal Tylenol use. This approach prioritizes both safety and necessity.
5. How can parents safely use Tylenol during pregnancy?
Use the lowest effective dose for the shortest time needed. Always consult a healthcare provider before prolonged use. Keep track of why and how often you take it. Context matters just as much as the medication itself.
6. What do biomarker studies reveal about Tylenol and autism?
Biomarker studies measure Tylenol directly in cord blood, reducing recall errors. Some have found dose-response patterns linking higher levels to higher autism risk. These findings are intriguing but still confounded by why the medication was needed. They add clues but not final answers.
7. Are there alternatives to Tylenol for pregnancy pain?
Some non-drug approaches include rest, hydration, and gentle physical therapy. In certain cases, guided cannabis-based therapies may help with related symptoms, but these require expert oversight. Discuss options openly with a knowledgeable clinician. Safety varies greatly depending on circumstances.
8. How do media headlines distort the science?
Headlines often simplify nuanced findings into fear-inducing statements. “Evidence consistent with association” becomes “Tylenol causes autism!” This fuels panic and guilt without improving understanding. Responsible communication is vital for families.
9. Should pregnant people completely avoid Tylenol?
No – not necessary. Completely avoiding Tylenol could lead to untreated fevers, which are dangerous for both parent and baby. Instead, use Tylenol thoughtfully and sparingly, guided by a clinician. Balance is key.
10. What is the future of research on Tylenol and autism?
The next frontier includes integrating biomarkers, genetics, and better tracking of fever and infection. Sibling studies and negative controls will play a major role. The goal is to finally untangle causation from correlation. Until then, careful interpretation is essential.