Why your body doesn’t respond to cannabis like it does to Zoloft, Tylenol, or a flu shot — and why that’s (usually) a good thing
Table of Contents
- The Trouble With the Old Model
- Cannabis Isn’t a Magic Pill—It’s More Like a Personal Trainer
- It Acts More Like Sleep, Nutrition, or Exercise Than a Pharmaceutical
- There Is No Standard Dose — And That’s On Purpose
- Patients Become Participants, Not Just Recipients
- Cannabis Doesn’t Work Despite Its Complexity—It Works Because of It
- The Old Model Is Broken Anyway
- The Future of Medicine May Look More Like Cannabis
- FAQ: How Cannabis Works Differently Than Traditional Medicine
- Q: Can cannabis replace my current medications?
- Q: How do I know which product to choose?
- Q: Is it really that different from traditional meds?
- Q: Why doesn’t cannabis come with a standard dose like my other medications?
- Q: How long does it take to notice an effect?
- Q: Why do effects vary so much between people?
- Q: Does cannabis treat the symptom or the system?
- Q: Isn’t cannabis just for pain or nausea?
- Q: Why do some doctors still hesitate to recommend it?
- Q: What’s the biggest misconception about cannabis as medicine?
TL;DR
- Cannabis isn’t a one-size-fits-all pill; it’s more like sleep or exercise—multi-system, multi-effect, and deeply personal. How cannabis works differently than traditional medicine should not be a secret!
- Traditional meds often target a single symptom. Cannabis supports balance across multiple systems at once.
- Context matters: sleep, stress, diet, and even time of day can change how cannabis works in your body.
- There’s no standard cannabis dose. Instead, patients are taught how to steer.
- It’s not broken medicine—it’s a better fit for real-life complexity.
The Trouble With the Old Model
Modern medicine likes clean lines and tidy labels. You have strep? Here’s penicillin. Broken bone? Cast. Insomnia? Ambien. Done and dusted.
But what if you don’t have one problem? What if your diagnosis reads more like a novel than a headline? Fatigue, pain, anxiety, digestive trouble, memory fog, emotional volatility—maybe even all at once? Welcome to the club.
For people living with complex or multidimensional conditions (think fibromyalgia, IBS, PTSD, chronic pain, autism, and yes, the tangle of stress that comes with modern life), traditional medicine often ends up throwing pills at parts of the problem—with mixed success and a full cabinet of side effects.
That’s where cannabis comes in. But let’s get one thing straight:
Cannabis Isn’t a Magic Pill—It’s More Like a Personal Trainer
If you’re looking for a single-molecule hammer to hit one nail, cannabis might frustrate you. But if you’re juggling sleep issues, mood dips, inflammatory pain, and general overwhelm, it starts to make a lot more sense.
Why? Because cannabis works across multiple systems at once. It gently nudges the endocannabinoid system (ECS), a kind of body-wide tuning fork that helps regulate mood, appetite, sleep, immune function, and more.
Think of it like this: if traditional medicine is a locksmith opening one stuck door, cannabis is more like an HVAC system restoring balance across the house.

It Acts More Like Sleep, Nutrition, or Exercise Than a Pharmaceutical
Here’s a fun experiment: try eating a bag of chips after a good night’s sleep, and then again after staying up all night. Same chips, completely different experience.
Cannabis is the same. Its effects depend not just on the product, but on the person using it and the context they’re in:
- Are you well-rested?
- Stressed?
- Fed or fasting?
- Hormones surging?
- Just exercised?
Every one of these factors changes how cannabis interacts with your body.
And just like nutrition or yoga or a long walk outside, the benefits of cannabis tend to build over time.
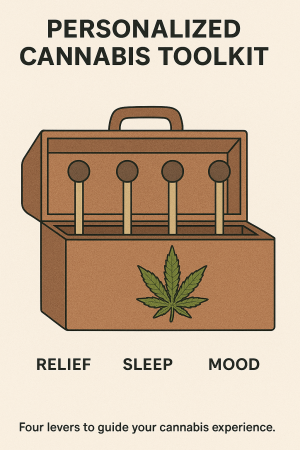
There Is No Standard Dose — And That’s On Purpose
Unlike pharmaceuticals that come pre-packaged in neatly color-coded blister packs, cannabis doesn’t offer a standard dose.
Why? Because standardization assumes a one-size-fits-all body. And spoiler: bodies aren’t standardized.
Instead of a prescription, patients get a toolkit—and they learn how to use it. The most effective cannabis clinicians teach people how to pull four main levers:
- Timing of onset (Do you need it to kick in now or later?)
- Duration of effect (How long do you want it to last?)
- Cognitive impact (Do you want mental clarity or mind-shifting effects?)
- Energy profile (Should it help you wind down or get going?)
Knowing how to work these levers means tailoring treatment to real-life needs, not lab-based averages.
Patients Become Participants, Not Just Recipients
When someone is handed a prescription, there’s usually a script that goes with it:
“Take one daily, with food, avoid alcohol, and call me in six months.”
With cannabis, it’s more like:
“Here’s how to recognize what your body is asking for. Here are the tools. Let’s experiment together.”
It’s a shift from compliance to curiosity. From being told what to take to learning how to navigate your own physiology. And yes, sometimes it feels a little like building IKEA furniture without the manual. But with good guidance, it’s empowering.
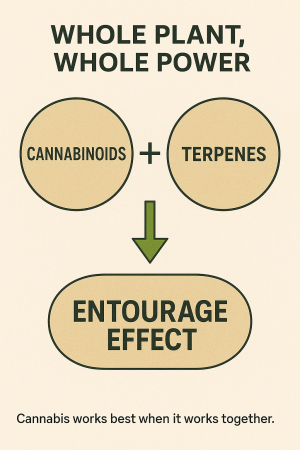
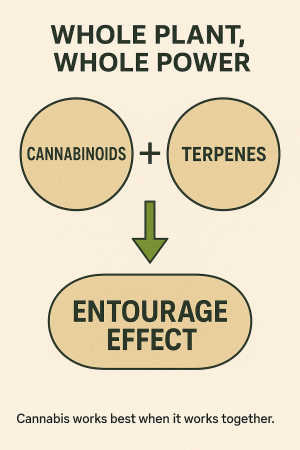
Cannabis Doesn’t Work Despite Its Complexity—It Works Because of It
People often ask: why don’t we just isolate the best part of cannabis and make it a pill?
We’ve tried. (Looking at you, Marinol.) But it rarely works as well as the whole plant.
That’s because cannabis is a symphony, not a solo act. Cannabinoids like THC and CBD play off each other. Terpenes (the fragrant oils that give strains their character) influence mood and effect. Even flavonoids may modulate how cannabis is absorbed and used.
Simplifying cannabis strips it of what makes it work.
The Old Model Is Broken Anyway
Let’s be honest: the traditional medical model isn’t doing great. It works wonders for acute emergencies, surgeries, and infectious diseases. But for chronic, complex conditions? Not so much.
It’s no wonder patients are turning to a medicine that asks different questions:
- What helps you feel like yourself again?
- What do you notice?
- How does this interact with the rest of your life?
Cannabis isn’t a cure-all. But it doesn’t pretend to be. It’s a tool that meets you where you are.
The Future of Medicine May Look More Like Cannabis
Here’s the real kicker: the things that make cannabis feel unusual today—personalized care, contextual effectiveness, multi-system action—are probably what all medicine should look like.
We don’t need more silver bullets. We need smart tools. Patient empowerment. Adaptive treatments. Doctors who listen. And yes, sometimes, a better night’s sleep.
Cannabis isn’t weird. It’s just ahead of the curve.
External Links:
Marijuana as a Substitute for Prescription Medications: A Qualitative Study
Good RX: What’s the Difference Between Medical Marijuana and Recreational Weed?
FAQ: How Cannabis Works Differently Than Traditional Medicine
Q: Can cannabis replace my current medications?
A: Not always, and not without guidance. Cannabis may reduce the need for certain meds, but should be introduced thoughtfully and with clinical oversight.
Q: How do I know which product to choose?
A: It depends on your goals. A good clinician will help you match product types to your needs—whether that’s better sleep, less anxiety, or more focus. Smart cannabis choices
Q: Is it really that different from traditional meds?
A: Yes. Not because it’s magical, but because it’s personal, adaptive, and system-wide. That’s what makes it powerful.
Q: Why doesn’t cannabis come with a standard dose like my other medications?
A: Because your endocannabinoid system is unique. Cannabis interacts with it differently in every person, so care has to be personalized—not one-size-fits-all. Cannabis dosing
Q: How long does it take to notice an effect?
A: It depends on the route (inhaled, oral, topical), your metabolism, and your condition. Effects can be felt in minutes or take days to build—timing matters.
Q: Why do effects vary so much between people?
A: Genetics, stress, diet, hormones, sleep, and other meds all influence how cannabis feels. The same product can work differently in the same person on different days.
Q: Does cannabis treat the symptom or the system?
A: Often both. Cannabis supports homeostasis by regulating underlying imbalances, not just masking symptoms like many conventional drugs.
Q: Isn’t cannabis just for pain or nausea?
A: Not at all. Research supports its use in anxiety, sleep, inflammation, cognition, seizures, appetite regulation, and more—thanks to its broad system-wide effects. Conditions that cannabis treats
Q: Why do some doctors still hesitate to recommend it?
A: Medical education has historically ignored the endocannabinoid system. Many clinicians simply haven’t been trained to work with it—yet. How to talk to your doctor about cannabis
Q: What’s the biggest misconception about cannabis as medicine?
A: That it’s recreational by nature. In reality, it can be one of the most precise, adaptable, and well-tolerated tools in modern care when used correctly.